Double Sequential AED
Double sequential defibrillation, also called double sequential external defibrillation (DSED) or dual sequential defibrillation, is an advanced resuscitation technique that has sparked growing debate in emergency medicine. Unlike standard defibrillation, which delivers a single shock from one defibrillator, DSED uses two defibrillators in rapid succession, sending electrical currents through the heart from different vectors.
The technique is considered for refractory ventricular fibrillation (VF), a dangerous, chaotic rhythm where the heart quivers instead of pumping blood. Refractory VF occurs when a patient does not respond after at least three standard shocks. Mortality rates in this group are extremely high, making it one of the most urgent and difficult problems in cardiac arrest management.
Because of this, clinicians and researchers are exploring whether DSED can improve survival and neurological outcomes in patients who fail to respond to conventional approaches. The 2022 DOSE-VF randomized trial suggested potential benefits, prompting a global debate on its viability as an advanced resuscitation technique.
 What is Double Sequential AED (DSED)?
What is Double Sequential AED (DSED)?
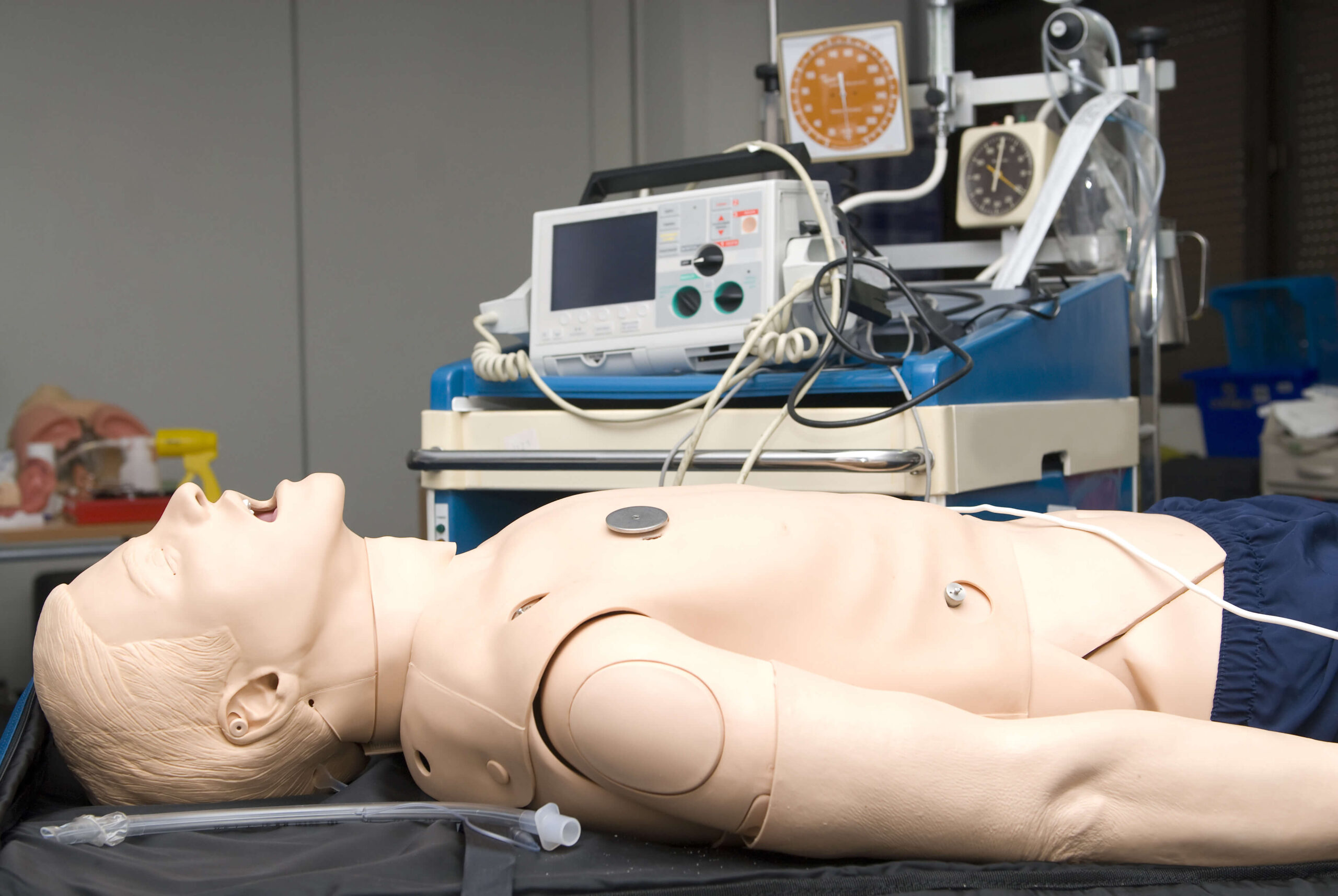
Double Sequential AED is an advanced technique that differs from the standard single-shock approach. In routine cardiac arrest care, one automated external defibrillator (AED) or manual defibrillator delivers a single electrical shock through pads placed on the chest. With DSED, however, two defibrillators are used in rapid sequence, delivering back-to-back shocks intended to stop chaotic electrical activity in the heart and allow a normal rhythm to resume.
How it Works: Mechanism of AED
DSED is based on the principle that refractory ventricular fibrillation may require more than a single vector of energy to reset the heart. Instead of one electrical pathway, two defibrillators create multiple shock vectors that increase the chances of depolarizing enough heart muscle to terminate fibrillation.
One set of pads is typically placed in the anterolateral position (below the right clavicle and on the left side of the chest). The second set is placed in an anteroposterior position (front and back), though other combinations are possible depending on equipment and clinical judgment.
Through these placements, the shocks travel through the heart from different directions, which is a concept known as vector change. This broader myocardial capture is what sets DSED apart from standard defibrillation, offering a potential advantage when conventional single shocks have failed.
Current Standing in Medical Guidelines
In 2023, the International Liaison Committee on Resuscitation updated its recommendations to acknowledge double sequential external defibrillation as a potential option for patients who remain in VF after three or more standard shocks. It was the first time a major resuscitation body has recognized DSED as a strategy worth considering in advanced cardiac arrest care.
That said, ILCOR’s language is measured. The recommendation is weak and based on low-certainty evidence, drawn primarily from a single randomized trial and limited observational data. ILCOR emphasizes that DSED should be seen as an emerging technique, not a proven standard.
Despite ILCOR’s acknowledgment, DSED has not been incorporated into the current Advanced Cardiac Life Support (ACLS) algorithms, and other resuscitation agencies remain cautious. Groups such as the European Resuscitation Council (ERC) have not recommended routine use of DSED, citing the limited evidence base, small sample sizes, and the logistical challenge of requiring two defibrillators in the field.
Standard defibrillation remains the cornerstone of shockable rhythm management, with DSED reserved for exceptional cases under local protocols. This underscores the need for caution: premature adoption without broad evidence may create inconsistency and confusion in resuscitation practice.
Dual Sequential Defibrillation Controversies & Safety Considerations
DSED has generated significant interest as an alternative strategy for refractory ventricular fibrillation, but it carries complex controversies and safety considerations that must be carefully weighed in clinical practice.
One key debate centers on whether DSED should involve simultaneous or sequential shocks. Simultaneous shocks, where two defibrillators fire exactly together, may risk electrical waveform overlap and even potential equipment damage. In contrast, sequential shocks delivered moments apart are thought to minimize such risks while still harnessing the theoretical benefit of dual energy vectors.
Other concerns include:
Replicability
While the landmark DOSE-VF trial demonstrated promising outcomes, it was conducted exclusively across six Canadian paramedic services. Whether such results can be replicated across different regions, ambulance systems, and patient populations remains an open question demanding further study.
Patient Risks
Using two defibrillators raises theoretical concerns about myocardial injury, as delivering higher cumulative energies or multiple shock vectors could potentially damage heart tissue.
Provider & Device Safety
Coordinating two defibrillators adds to the complexity of care in high-stress arrest situations. There is potential for synchronization errors that could endanger both patient and equipment.
Spotlight: The DOSE-VF Trial (2022)
The landmark DOSE-VF cluster-randomized trial compared three strategies – standard defibrillation, vector-change (VC) defibrillation, and DSED – in adults with refractory VF during out-of-hospital cardiac arrest.
The trial enrolled 405 patients across six Canadian paramedic services using a cluster crossover design. Patients in VF after three standard shocks were randomized by paramedic service to one of the three defibrillation strategies.
Key Outcomes:
- Survival to hospital discharge: 30.4% with DSED vs. 13.3% with standard defibrillation
- DSED also outperformed standard defibrillation in ROSC rates (46.4% vs. 26.5%) and neurologically favorable surviva27.4% vs. 11.2%
Unfortunately, the trial was halted early due to the COVID-19 pandemic, enrolling only 405 of the planned 930 patients, which has raised concerns about the validity of the statistics and an overestimation of benefits. The cluster design also introduces risk of imbalance and confounding, while analysis tools may not fully adjust for multiplicity.
Despite these limitations, DOSE-VF remains the most robust evidence to date, clearly signaling that DSED merits further investigation while stopping short of cementing it as standard care.
When to Use Double Sequential AED
DSED is a rescue strategy best considered in scenarios such as: witnessed OHCA with early CPR and persistent VF after three shocks; recurrent VF despite transient ROSC where vector change hasn’t helped; or prolonged arrests where high-quality basics are intact but the rhythm remains stubbornly shockable.
Prehospital use (EMS): Deployment in the field depends on having two defibrillators available and a team trained to coordinate charging and sequential delivery without prolonging hands-off time.
In-hospital use: Hospitals provide a more controlled environment with advanced monitoring and rapid confirmation of refractory versus recurrent VF. Ready access to additional defibrillators and post-shock assessment can streamline delivery, but teams should still pre-assign roles, rehearse the AED sequence, and document settings and timing.
Across settings, the decision to use DSED should proceed only when sequential shocks can be delivered with minimal interruption, after first-line measures are optimized, and within established protocols.
 Double Sequence Defibrillation: Step-by-Step
Double Sequence Defibrillation: Step-by-Step
The following guide reflects the method described in the ILCOR draft Consensus on Science and Treatment Recommendations (CoSTR, 2023), as well as the protocol used in the DOSE-VF randomized trial. It represents the best currently available evidence for how double sequential external defibrillation should be performed in cases of refractory ventricular fibrillation.
Step 1: Prepare Equipment
Obtain two defibrillators, each with its own set of pads. Confirm both devices are functioning and can deliver biphasic shocks at standard energy (typically 200 J).
Step 2: Apply Pads
Place the first set of pads in the standard anterolateral position (below the right clavicle and the left lateral chest). Place the second set in the anteroposterior position (front of chest and back), taking care that pads do not overlap so as to prevent electrical feedback between devices.
Step 3: Charge Both Defibrillators
Charge the devices to the recommended biphasic energy setting (typically 200 joules each), unless device-specific protocols suggest otherwise.
Step 4: Deliver Sequential Shocks
Designate one operator to trigger both shocks in rapid sequence, pressing the shock buttons milliseconds apart.
Step 5: Resume Chest Compressions
Resume chest compressions immediately after shocks, keeping pre- and post-shock pauses under 10 seconds. Reassess rhythm at the next pulse check per standard ACLS protocol.
Step 6: Repeat or Transition if Needed
If ventricular fibrillation persists, follow local protocols regarding repeat attempts or transition to alternative therapies. Then, continue advanced post-resuscitation care if ROSC is achieved.
Guidelines & Ethical Considerations
Despite the inclusion of DSED in ILCOR’s 2023 draft recommendations, the language reflects uncertainty in that the recommendation is weak, supported by low-certainty evidence, and clearly framed as conditional rather than definitive.
This careful stance highlights the ethical balance between innovation and protocol adherence. On one hand, DSED offers hope in scenarios where conventional methods almost always fail, raising the possibility of saving lives otherwise lost. On the other, introducing a complex intervention prematurely risks undermining standardized training and protocols that guide thousands of responders worldwide.
Practical limitations deepen the ethical debate. DSED requires two defibrillators, a resource not always available in the field. Paramedic crews may only have access to one device, and coordinating the arrival of a second unit introduces delays that could cancel out any potential benefit. In hospitals, where additional devices are on hand and advanced monitoring is available, DSED is easier to perform safely, but even there, many providers have not been trained in the technique. The training gap among medics, nurses, and physicians is real and raises questions about whether the procedure should be promoted before widespread education and competency programs are in place.
There is also the question of positioning DSED as a “last-resort” intervention versus a mainstream strategy. Some experts argue that it should only be attempted when all standard measures are exhausted, treating it as an experimental maneuver for otherwise unsalvageable arrests. Until further large-scale studies replicate the survival benefits seen in the DOSE-VF trial, most guideline committees are holding to the conservative view: DSED is worth exploring, but not ready for widespread inclusion in core algorithms.
The Future of Double Sequential AED
As resuscitation science evolves, researchers are already asking what lies beyond double sequential shocks. Some experimental systems have explored triple-sequential protocols, though these remain highly theoretical and far from clinical practice. Meanwhile, device manufacturers such as Zoll and others are examining whether advances in defibrillator technology could automate vector change or sequence delivery, reducing the complexity of coordinating multiple devices in real time.
What remains clear is that the field faces major research gaps. The DOSE-VF trial provided important early evidence, but further randomized controlled trials are needed to validate its findings across different EMS systems, hospitals, and patient populations. Equally important are studies on long-term safety outcomes, including myocardial injury risk, neurological recovery, and device performance over time.
Finally, the challenge of global adoption looms large. Systems with limited resources may struggle to deploy two defibrillators at every arrest, while regions with advanced infrastructure will need training programs and protocols to ensure consistency. The next decade will likely determine whether DSED becomes a mainstream intervention or remains a specialized, last-resort measure.
Frequently Asked Questions
Where do you place the pads for DSED?
One set is placed in the standard anterolateral position and the second in the anteroposterior position to create different shock vectors.
How many joules do you use?
Each defibrillator is typically charged to the standard biphasic setting, usually 200 J.
Is triple-sequential defibrillation real?
It has been described in experimental discussions, but there is no evidence or guideline support for using three defibrillators in practice.
What is DSED in ACLS?
Currently, DSED is not part of the ACLS algorithm. It is considered an experimental or last-resort strategy for refractory VF, and its use depends on local protocols.
Balancing Promise With Caution
Early evidence suggests DSED may improve outcomes in otherwise fatal cases of refractory ventricular fibrillation, but its role remains unsettled. The evidence base is still small, and major resuscitation bodies outside ILCOR have not endorsed it for routine use.
For now, DSED should be viewed as a promising but experimental strategy, not a replacement for proven interventions. Clinicians should stay informed as new research emerges and practice within the bounds of their system’s training and oversight. Above all, always follow the latest ACLS and EMS protocols in your region, and consult with your medical director before attempting emerging techniques like DSED.

