ECG Rhythms
About this Resource
ACLS is the preeminent course for healthcare professionals responsible for providing advanced cardiac care to patients in various in-facility and prehospital settings. Designed by experienced providers in conjunction with board-certified physicians and veteran ACLS instructors, this resource serves as an engaging and comprehensive approach to reviewing the core rhythms of ACLS practice.
The resource reviews the pathophysiology, defining criteria and ECG features, clinical manifestations, common etiologies, and ECG presentation for the 15 core rhythms, including ventricular fibrillation, accessory-mediated supraventricular tachycardia, and several atrioventricular blocks.
Recognition of Cardiac Arrest: Ventricular Fibrillation (VFib)
Pathophysiology
- The ventricles consist of areas of normal myocardium alternating with regions of ischemic, injured, or infarcted tissue, leading to a chaotic asynchronous ventricular depolarization and repolarization pattern. Without organized ventricular depolarization, the ventricles cannot contract as a unit, halting cardiac output and causing the heart to quiver and seize pumping blood
Defining Criteria and ECG Features
- Rate: Uncountable. Electrical deflections are very rapid and too disorganized to count. Baseline undulations occur between 150-500 per minute.
- QRS Complex: No recognizable QRS complex exists, and regular negative-positive-negative patterns cannot be observed.
- Rhythm: Indeterminate. No regular rhythmic patterns can be discerned upon analysis, and electrical waveforms vary in size and shape with a profoundly disorganized pattern of sharp deflections.
- Amplitude: Measured from peak to trough and used to subjectively characterize VFib as either fine (2-5 mm), medium or moderate (5-10 mm), coarse (10-15 mm), or very coarse (>15 mm).
Clinical Manifestations
- Pulse disappears with the onset of VFib but may disappear beforehand if it is preceded by rapid ventricular tachycardia (VTach); pulseless VTach degrades rapidly into VFib and is therefore considered cardiac arrest.
- Physical collapse and unresponsiveness.
- Agonal gasps or apnea.
- Sudden death.
Common Etiologies
- Acute coronary syndrome that has led to ischemic areas of myocardial tissue.
- Untreated VTach (stable and unstable).
- Premature ventricular complexes (PVCs) with the R-on-T phenomenon.
- Drug, electrolyte, or acid-base abnormalities that prolong the relative refractory period.
- Primary or secondary QT prolongation.
- Electrocution or hypoxia.
ECG Presentation

Figure 1. Ventricular Fibrillation. Presented at a rate of zero beats per minute (no pulse). Note the high-amplitude waveforms, which vary in size, shape, and rhythm, representing chaotic ventricular electrical activity.
Recognition of Cardiac Arrest: Pulseless Electrical Activity (PEA)
Pathophysiology
- Cardiac conduction impulses occur in an organized pattern but do not produce myocardial contraction; this condition was formerly called electromechanical dissociation. There is insufficient ventricular filling during diastole or ineffective contractions.
Defining Criteria and ECG Features
- Rate: Can be fast (>100 beats per minute) or slow (<60 beats per minute).
- QRS Complex: Can be narrow (<0.12 seconds) or wide (>0.12 seconds).
- Rhythm: Organized electrical activity, but less so compared to normal sinus rhythm.
Clinical Manifestations
- Physical collapse and unresponsiveness.
- Agonal gasps or apnea.
- No pulse detectable by palpation.
- Low systolic blood pressure could still be present.
Common Etiologies
- Use the H’s and T’s mnemonic to recall possible underlying causes:
- Hypovolemia
- Hypoxia
- Hydrogen ion (acidosis)
- Hypo-/hyperkalemia
- Hypothermia
- Tension pneumothorax
- Tamponade, cardiac
- Toxins (i.e., drug overdose, ingestion
- Thrombosis, pulmonary (embolism)
- Thrombosis, coronary (ACS)
- Narrow QRS and fast heart rate are caused mainly by a non-cardiac etiology; wide QRS and slow heart rate are caused primarily by a cardiac etiology.
ECG Presentation
PEA can look like any rhythm that is characterized by organized electrical activity but is accompanied by the absence of a palpable pulse. For example, the ECG monitor can reflect a sinus rhythm (e.g., sinus bradycardia, sinus tachycardia, etc.), but no palpable pulse is present. In this case, the rhythm can be identified as PEA.
Recognition of Cardiac Arrest: Asystole
Pathophysiology
- Asystole can be primary or secondary. Primary asystole occurs when the heart’s electrical system fails to generate a ventricular depolarization, which may result from ischemia or degeneration (i.e., sclerosis) of the sinoatrial (SA) or atrioventricular (AV) node conducting systems. Secondary asystole occurs when factors outside of the heart’s electrical conduction system result in a failure to generate any electrical depolarization.
Defining Criteria and ECG Features
- Rate: No ventricular activity is observed.
- QRS Complex: There are no visible deflections consistent with a QRS complex.
- Rhythm: No ventricular activity is observed.
- PR Interval: Cannot be determined. Occasionally, the P-wave is seen, but the R wave must be absent for the rhythm to be truly asystolic.
Clinical Manifestations
- Physical collapse and unresponsiveness.
- Early agonal gasps or apnea.
- No pulse or blood pressure.
- Death.
Common Etiologies
- End of life (death).
- Cardiac ischemia.
- Acute respiratory failure or hypoxia.
- Massive electrical shock (e.g., electrocution, lightning strike).
- May represent “stunning” of the heart immediately after defibrillation before the resumption of spontaneous rhythm.
ECG Presentation
Asystole is often preceded by QRS-like complexes that represent a minimum of electrical activity, probably ventricular escape beats. These are followed by a long section in which electrical activity is absent, where the patient is now pulseless and unresponsive. This point can now be identified as asystole.
Recognition of Bradyarrhythmias: Sinus Bradycardia
Pathophysiology
- Impulses originate at the SA node at a slow rate. It may be physiologic. It can be a physical sign, as in sinus tachycardia.
Defining Criteria and ECG Features
- Regular P-waves followed by regular QRS complexes at a rate of <60 beats per minute. Often a physical sign rather than an abnormal rhythm.
- Rate: <60 beats per minute. When symptomatic, the rate is generally <50 beats per minute.
- QRS Complex: Narrow, <0.12 seconds (often <0.11 seconds) in the absence of an intraventricular conduction defect.
- Rhythm: Regular sinus.
- PR Interval: Regular, 0.12 to 0.20 seconds.
- P-waves: Size and shape normal. A QRS complex follows every P-wave, and a P-wave precedes every QRS complex.
Clinical Manifestations
- The person is usually asymptomatic when at rest.
- With increased activity and sinus node dysfunction, a constant slow rate can lead to symptoms of easy fatigue, shortness of breath, dizziness or light-headedness, syncope, hypotension, diaphoresis, pulmonary congestion, and frank pulmonary edema.
- The ECG can independently display acute ST-segment or T-wave deviation or ventricular arrhythmias.
Common Etiologies
- It can be expected for well-conditioned people.
- A vasovagal event, such as vomiting, Valsalva maneuver, rectal stimuli, inadvertent pressure on carotid sinus (shaver’s syncope)
- Acute coronary syndromes that affect circulation to the SA node (right coronary artery), most often inferior acute myocardial infarctions (AMIs).
- Adverse drug effects (e.g., beta-blockers or calcium channel blockers, digoxin, quinidine)
ECG Presentation

Figure 2. Sinus Bradycardia. Presented at a rate of approximately 50 beats per minute. Note the normal sinus rhythm presentation, but at an abnormally lower rate resulting in a slower production of deflections.
Recognition of Tachyarrhythmias: Sinus Tachycardia
Pathophysiology
- More of a physical response than an actual arrhythmia or pathologic condition. Normal impulse formation and conduction.
Defining Criteria and ECG Features
- Rate: >100 beats per minute.
- QRS Complex: May be regular or wide if there is an underlying abnormality. There is a P-wave for every QRS complex.
- Rhythm: Regular sinus.
- PR Interval: Usually <0.20 seconds.
Clinical Manifestations
- Nonspecific for tachycardia.
- Symptoms may be present due to the cause of the tachycardia (fever, hypovolemia, etc.).
Common Etiologies
- Normal exercise, adrenergic stimulation, pain, or anxiety.
- Clinical conditions including hypoxemia, fever, hypovolemia, hyperthyroidism, and anemia.
ECG Presentation

Figure 3. Sinus Tachycardia. Presented at a rate of approximately 140 beats per minute. Note the normal sinus rhythm presentation, but at an abnormally higher rate resulting in a faster production of deflections.
Recognition of Tachyarrhythmias: Atrial Fibrillation
Pathophysiology
- Atrial impulses are faster than sinoatrial (SA) node impulses. Impulses take multiple chaotic, random pathways through the atria.
Defining Criteria and ECG Features
- Irregularly irregular rhythm with variation in both interval and amplitude from R-wave to R-wave. Usually dependable and can also be observed in multifocal atrial tachycardia (MAT).
- Rate: Wide-ranging ventricular response to atrial undulations between 300 and 400 per minute. It May be normal or slow if atrioventricular (AV) nodal conduction is abnormal (e.g., sick sinus syndrome).
- QRS Complex: Remains <0.12 seconds unless QRS complex is distorted by fibrillation, flutter waves, or conduction defects through the ventricles.
- Rhythm: Irregular (i.e., irregularly irregular).
- PR Interval: Cannot be measured.
- P-waves: Only chaotic atrial fibrillatory waves are observed.
Clinical Manifestations
- Signs and symptoms are a function of the ventricular response rate to atrial fibrillation waves: “atrial fibrillation with a rapid ventricular response may be characterized by dyspnea on exertion, shortness of breath, and sometimes acute pulmonary edema.
- Loss of “atrial kick” may lead to a drop in cardiac output and decreased coronary perfusion.
- Irregular rhythm is often perceived as “palpitations.”
- Atrial fibrillation and atrial flutter can be asymptomatic.
Common Etiologies
- Acute coronary syndromes, coronary artery disease, or congestive heart failure.
- Diseased mitral or tricuspid valve.
- Hypoxia, acute pulmonary embolism.
- Drug-induced: digoxin, quinidine, beta-agonists, theophylline.
- Clinical conditions including sepsis, hypertension, and hyperthyroidism.
ECG Presentation

Figure 4. Atrial fibrillation. Presented at a rate of approximately 90 beats per minute. Note how the P-waves are absent, coarse fibrillatory waves can frequently be seen, and there is difficulty in identifying atrial activity. The QRS complexes are also irregularly irregular with varying R-R intervals.
Recognition of Tachyarrhythmias: Atrial Flutter
Pathophysiology
- Atrial impulses are faster than sinoatrial (SA) node impulses. Impulses take a circular course around the atria, setting up flutter waves.
Defining Criteria and ECG Features
- Rate: Atrial rate is 220-350 beats per minute. Ventricular response is a function of AV node block or conduction of atrial impulses. Ventricular response is near>150-180 beats per minute because of AV nodal conduction limits.
- QRS Complex: Remains <0.12 seconds unless QRS complex is distorted by fibrillation, flutter waves, or conduction defects through the ventricles.
- Rhythm: Regular. Ventricular rhythm is often regular. Set ratio to atrial rhythm, e.g., 2:1 or 4:1.
- PR Interval: Cannot be measured.
- P-waves: No true P-waves are observed.
Clinical Manifestations
- Signs and symptoms are a function of the ventricular response rate to atrial fibrillation waves: “atrial fibrillation with a rapid ventricular response may be characterized by dyspnea on exertion, shortness of breath, and sometimes acute pulmonary edema.
- Loss of “atrial kick” may lead to a drop in cardiac output and decreased coronary perfusion.
- Irregular rhythm is often perceived as palpitations.
- Atrial fibrillation and atrial flutter can be asymptomatic.
Common Etiologies
- Acute coronary syndromes, coronary artery disease, or congestive heart failure.
- Diseased mitral or tricuspid valve.
- Hypoxia, acute pulmonary embolism.
- Drug-induced: digoxin, quinidine, beta-agonists, theophylline.
- Clinical conditions including sepsis, hypertension, and hyperthyroidism.
ECG Presentation

Figure 5. Atrial Flutter. Presented at a rate of approximately 75 beats per minute. Note the flutter waves in classic sawtooth pattern.
Recognition of Supraventricular Tachyarrhythmias: Accessory-Mediated Supraventricular Tachycardia (SVT)
Pathophysiology
- Re-entry phenomenon: Impulses repeatedly recycle in the AV node because an abnormal rhythm circuit allows a wave of depolarization to travel in a circle. Usually, the depolarization travels antegrade (forward) through the abnormal pathway and then loops back retrograde through the “normal” conduction tissues. Accessory-mediated SVT may include AV nodal reentrant tachycardia or AV reentry tachycardia.
Defining Criteria and ECG Features
- Characterized as regular, narrow-complex tachycardia without P-waves and sudden onset or cessation. Some experts require capturing the abrupt onset or cessation on a monitor strip to merit the diagnosis of reentry SVT.
- Rate: Exceeds the upper limit of sinus tachycardia at rest (>220 beats per minute), seldom <150 beats per minute, often up to 250 beats per minute.
- QRS Complex: Normal and narrow.
- Rhythm: Regular.
- P-waves: Infrequently seen because rapid rate causes P-waves to be hidden in preceding T-waves; challenging to detect because the origin is low in the atrium.
Clinical Manifestations
- Palpitations felt by the patient at onset; becomes anxious and uncomfortable.
- Low exercise tolerance with very high rates.
- Symptoms of unstable tachycardia may occur.
Common Etiologies
- Accessory conduction pathway occurs in many patients with SVT.
- For otherwise healthy people, many factors can provoke SVT re-entry: caffeine, hypoxia, cigarettes, stress, anxiety, sleep deprivation, and numerous medications.
- Frequency of SVT increases in unhealthy patients with coronary artery disease, chronic obstructive pulmonary disease, and congestive heart failure.
ECG Presentation

Figure 6. Accessory-Mediated Supraventricular Tachycardia. Presented at a rate of approximately 180 beats per minute. Note that sinus rhythm can often present with spontaneous reentry SVT.
Recognition of Ventricular Tachyarrhythmias: Monomorphic Ventricular Tachycardia (VTach)
Pathophysiology
- Impulse conduction is slowed around areas of ventricular injury, infarct, or ischemia. These areas of injury can cause the impulse to take a circular course, leading to the re-entry phenomenon and rapid repetitive depolarizations, while also serving as sources of ectopic impulses (irritable foci).
Defining Criteria and ECG Features
- The same morphology is seen in every QRS complex. Three or more consecutive premature ventricular contractions (PVCs) indicate VTach, where anything <30 seconds duration is non-sustained and anything >30 seconds duration is sustained.
- Rate: Ventricular rate >100 beats per minute. Typically, the ventricular rate is 120-250 beats per minute.
- QRS Complex: Wide and bizarre, “PVC-like” complexes 0.12 seconds, with a large T-wave of opposite polarity from QRS.
- Rhythm: Regular ventricular rhythm.
- PR Interval: Nonexistent (rhythm is AV dissociated).
- P-waves: Infrequent but seen; VTach is a form of AV dissociation, a defining characteristic for wide-complex tachycardias of ventricular origin versus supraventricular tachycardias with aberrant conduction.
Clinical Manifestations
- Typically, symptoms of decreased cardiac output (orthostasis, hypotension, syncope, signs of inadequate perfusion, etc.) will develop.
- Monomorphic VTach can be asymptomatic despite the widespread belief that sustained VTach always produces symptoms.
- Untreated and sustained VTach will deteriorate to unstable VTach and often to VFib.
Common Etiologies
- An acute ischemic event with areas of ventricular irritability leading to PVCs.
- Low ejection fraction due to chronic systolic heart failure.
- PVCs occur during the relative refractory period of the cardiac cycle (R-on-T phenomenon).
- Drug-induced prolonged QT interval (tricyclic antidepressants, procainamide, sotalol, amiodarone, ibutilide, dofetilide, some antipsychotics, digoxin, some long-acting antihistamines, certain antibiotics).
ECG Presentation
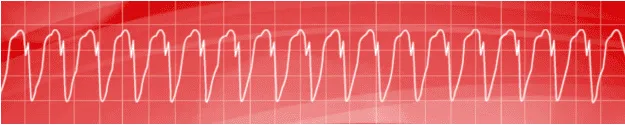
Figure 7. Monomorphic Ventricular Tachycardia. Presented at a rate of approximately 210 beats per minute. Note the wide QRS complexes with T-waves of opposite polarity.
Recognition of Ventricular Tachyarrhythmias: Polymorphic Ventricular Tachycardia (VTach)
Pathophysiology
- Impulse conduction is slowed around areas of ventricular injury, infarct, or ischemia. These areas of injury can cause the impulse to take a circular course, leading to the re-entry phenomenon and rapid repetitive depolarizations, while also serving as sources of ectopic impulses (irritable foci).
Defining Criteria and ECG Features
- Recognizable variation and inconsistency seen in QRS complex morphology
- Rate: Ventricular rate >100 beats per minute. Typically, the ventricular rate is 120-250 beats per minute.
- QRS Complex: Wide and bizarre, “PVC-like” complexes 0.12 seconds, with a large T-wave of opposite polarity from QRS.
- Rhythm: Regular or irregular ventricular rhythm with no atrial activity.
- PR Interval: Nonexistent (rhythm is AV dissociated).
- P-waves: Infrequent but present; VTach is a form of AV dissociation, a defining characteristic for wide-complex tachycardias of ventricular origin versus supraventricular tachycardias with aberrant conduction.
Clinical Manifestations
- Typically, symptoms of decreased cardiac output (orthostasis, hypotension, syncope, signs of inadequate perfusion, etc.) will develop.
- Untreated and sustained VTach will deteriorate to unstable VTach and often to VFib.
Common Etiologies
- An acute ischemic event with areas of ventricular irritability leading to PVCs.
- PVCs occur during the relative refractory period of the cardiac cycle (R-on-T phenomenon).
- Drug-induced prolonged QT interval (tricyclic antidepressants, procainamide, sotalol, amiodarone, ibutilide, dofetilide, some antipsychotics, digoxin, some long-acting antihistamines, certain antibiotics).
- Hereditary long QT interval syndromes.
ECG Presentation
Polymorphic ventricular tachycardia will have a similar presentation to monomorphic ventricular tachycardia, with the exception that the QRS complexes display multiple differentiating morphologies.
Recognition of Ventricular Tachyarrhythmias: Torsades de Pointes
Pathophysiology
- Torsades de Pointes is a unique subtype of polymorphic VTach
- The QT interval is abnormally long during a baseline ECG, leading to an increase in the relative refractory period of the cardiac cycle. This increases the probability that a PVC will occur on the T-wave (i.e., R-on-T phenomenon), often inducing VTach via the R-on-T phenomenon.
Defining Criteria and ECG Features
- QRS complexes display a spindle-node pattern in which VTach amplitude increases and then decreases in a regular pattern, creating the spindle. The initial deflection at the start of one spindle will be followed by complexes of opposite deflection at the start of the next spindle, creating the node.
- Rate: Atrial rate cannot be determined. The ventricular rate fluctuates between 150 to 250 complexes per minute.
- QRS Complex: Classic spindle-node pattern.
- Rhythm: Irregular ventricular rhythm.
- PR Interval: Nonexistent.
- P-waves: Nonexistent.
Clinical Manifestations
- The tendency toward sudden deterioration to pulseless VTach or VFib.
- Typically, symptoms of decreased cardiac output (orthostasis, hypotension, syncope, signs of inadequate perfusion, etc.) will develop.
Common Etiologies
- Most commonly occurs in patients with prolonged QT intervals.
- Drug-induced prolonged QT interval (e.g., tricyclic antidepressants, procainamide, sotalol, amiodarone, ibutilide, dofetilide, some antipsychotics, digoxin, some long-acting antihistamines, and certain antibiotics).
- Electrolyte and metabolic alterations result in inherited forms of long QT syndrome or acute ischemic events.
ECG Presentation
Torsades de Pointes is characterized by the start of a spindle that is identified by a negative initial deflection and increasing QRS amplitude, followed by a node and preceded by a second spindle. Here, a positive initial deflection and spindling in QRS amplitude will be observed, and the pattern will continuously repeat until the rhythm likely deteriorates to an easily identifiable VTach or VFib.
Recognition of AV Blocks: First-Degree AV Block
Pathophysiology
- Impulse conduction is slowed at the AV node for a fixed interval creating a partial block. It may be a sign of a secondary problem or a primary conduction abnormality.
Defining Criteria and ECG Features
- Rate: First-degree AV block can be seen with normal sinus mechanisms (60-100 beats per minute) but also sinus bradycardia (<60 beats per minute) and sinus tachycardia (>100 beats per minute).
- QRS Complex: Narrow, <0.12 seconds in absence of intraventricular conduction defect.
- Rhythm: Regular sinus.
- PR Interval: Prolonged (>0.20 seconds) but fixed.
- P-waves: Size and shape normal. A QRS complex follows every P-wave, and a P-wave precedes every QRS complex.
Clinical Manifestations
- Classically asymptomatic.
Common Etiologies
- Many first-degree AV blocks occur due to drugs, particularly the AV nodal blockers (e.g., beta-blockers, nondihydropyridine calcium channel blockers, digoxin).
- Any condition that stimulates the parasympathetic nervous system (e.g., vasovagal reflex).
- Acute coronary syndromes that affect circulation to the SA node (right coronary artery), most often inferior acute myocardial infarctions (AMIs).
ECG Presentation

Figure 8. First-Degree AV Block. Presented at a rate of approximately 70 beats per minute. Note how the PR intervals are prolonged but fixed. Here, there is no disruption of atrial to ventricular conduction. This patient would generally be asymptomatic, and the rhythm would only be discovered on a routine ECG.
Recognition of AV Blocks: Second-Degree AV Block Type I (Mobitz I, Wenckebach)
Pathophysiology
- The site of pathology is the AV node, whose blood supply comes from branches of the right coronary artery. Impulse conduction is progressively slowed at the AV node, increasing the PR interval until one sinus impulse is completely blocked and the QRS complex fails to follow.
Defining Criteria and ECG Features
- Rate: The atrial rate is just slightly faster than the ventricular rate because of a drop in electrical conduction. However, the rates themselves are usually within the normal range.
- QRS Complex: Usually <0.12 seconds, but a complex will periodically drop out.
- Rhythm: Atrial complexes are regular and ventricular complexes are irregular in timing because of dropped beats; they can show regular P-waves marching through irregular QRS.
- PR Interval: Progressive lengthening of PR interval occurs from cycle to cycle, with a P-wave lacking a subsequent QRS complex (i.e., dropped beat).
- P-waves: Size and shape normal. A QRS complex is periodically dropped after a single P-wave (i.e., dropped beat).
Clinical Manifestations
- Often occurs secondary to sinus bradycardia.
- Most often asymptomatic, but presenting symptomatology includes chest pain, shortness of breath, and decreased level of consciousness.
- Likely accompanied by hypotension, shock, pulmonary congestion, congestive heart failure, and angina.
Common Etiologies
- AV nodal blocking agents (e.g., beta-blockers, nondihydropyridine calcium channel blockers, digoxin).
- Conditions that stimulate the parasympathetic nervous system.
- The acute coronary syndrome involves the right coronary artery.
ECG Presentation

Figure 9. Second-Degree AV Block Type I. Presented at a rate of approximately 50 beats per minute. Note the progressive lengthening of the PR interval until one P-wave is not followed by a QRS complex. Here, the conduction of an impulse through the AV node is blocked, resulting in the absence of the QRS complex.
Recognition of AV Blocks: Second-Degree AV Block Type II (Mobitz II, Infranodal)
Pathophysiology
- The site of the block is most often below the AV node at the bundle of His or at the bundle branches. Impulse conduction is normal through the node. Thus no first-degree block and no prior PR prolongation.
Defining Criteria and ECG Features
- Rate: Atrial rate is usually 60-100 beats per minute. The ventricular rate is, by definition, because of blocked impulses, slower than the atrial rate with fluctuation.
- QRS Complex: Narrow (<0.12 seconds) implies high block relative to AV node, whereas wide (0.12 seconds) implies low block relative to AV node.
- Rhythm: Atrial is regular, but ventricular is irregular. The ventricular rate is only regular if there is a consistent 2:1 or 3:1 block.
- PR Interval: Constant with no progressive prolongation as with Type I second-degree AV block Mobitz, which is a distinguishing characteristic.
- P-waves: Typical in size and shape, though some P waves will not be conducted and therefore not followed by a QRS complex.
Clinical Manifestations
- Often occurs secondary to sinus bradycardia.
- Presenting symptomatology includes chest pain, shortness of breath, and decreased level of consciousness.
- Likely accompanied by hypotension, shock, pulmonary congestion, congestive heart failure, and acute myocardial infarction (AMI).
Common Etiologies
- The acute coronary syndrome involves branches of the left coronary artery.
ECG Presentation

Figure 10. Second-Degree AV Block Type II. Presented at a rate of approximately 60 beats per minute. Note the regular PR-QRS intervals until two dropped beats occur; borderline normal QRS complexes indicate high nodal block.
Recognition of AV Blocks: Third-Degree AV Block
Pathophysiology
- Injury or damage to the cardiac conduction system so that no impulses pass between the atria and the ventricles, neither antegrade nor retrograde, resulting in a complete block. This can occur in several anatomic areas including the AV node, the bundle of His, and bundle branches.
Defining Criteria and ECG Features
- Rate: The atrial rate is usually 60-100 beats per minute with impulses being completely independent of the slower ventricular rates, which depend on the rate of ventricular escape beats that arise. A ventricular escape rate that is slower than the atrial rate is a third-degree AV block at roughly 20-40 beats per minute. A ventricular escape rate that is faster than the atrial rate is AV dissociate at roughly 40-55 beats per minute.
- QRS Complex: Narrow (<0.12 seconds) implies high block relative to AV node, whereas wide (0.12 seconds) implies low block relative to AV node.
- Rhythm: Both the atrial and ventricular rhythms are regular but dissociated.
- PR Interval: There is no observable relationship between the P-waves and R-waves.
- P-waves: Typical in size and shape.
Clinical Manifestations
- Often occurs secondary to sinus bradycardia.
- Presenting symptomatology includes chest pain, shortness of breath, and decreased level of consciousness.
- Likely accompanied by hypotension, shock, pulmonary congestion, congestive heart failure, acute myocardial infarction (AMI).
Common Etiologies
- The acute coronary syndrome involves branches of the left coronary artery.
- Involves left anterior descending (LAD) artery and branches to the interventricular septum (supply bundle branches).
ECG Presentation
Figure 11. Third-Degree AV Block. Presented at a rate of approximately 40 beats per minute. Note regular P-waves at 50-55 beats per minute and regular ventricular escape beats at 35-40 beats per minute, but no visible relationship between P-waves and escape beats.

