Bradycardia Algorithm
Effective management of bradycardia in pediatric patients is crucial for emergency care professionals. Understanding the PALS bradycardia algorithm enables providers to quickly assess and treat life-threatening slow heart rhythms in children. This guide offers an overview of the key aspects of the PALS bradycardia algorithm, enhancing your ability to respond promptly during critical situations.
Importance of the PALS Bradycardia Algorithm
The PALS bradycardia algorithm is a systematic approach designed to assist clinicians in identifying and managing bradycardia in pediatric patients. It focuses on:
- Early Recognition: Promptly identifying signs of bradycardia to initiate immediate intervention.
- Assessment of Hemodynamic Stability: Determining the impact of bradycardia on circulation and organ perfusion.
- Appropriate Intervention: Implementing correct treatments based on the severity and underlying cause of the bradycardia.
By adhering to the PALS bradycardia algorithm, health care providers can improve patient outcomes and reduce the risk of progression to cardiac arrest.
Pediatric Bradycardia with Pulse/Poor Perfusional Algorithm
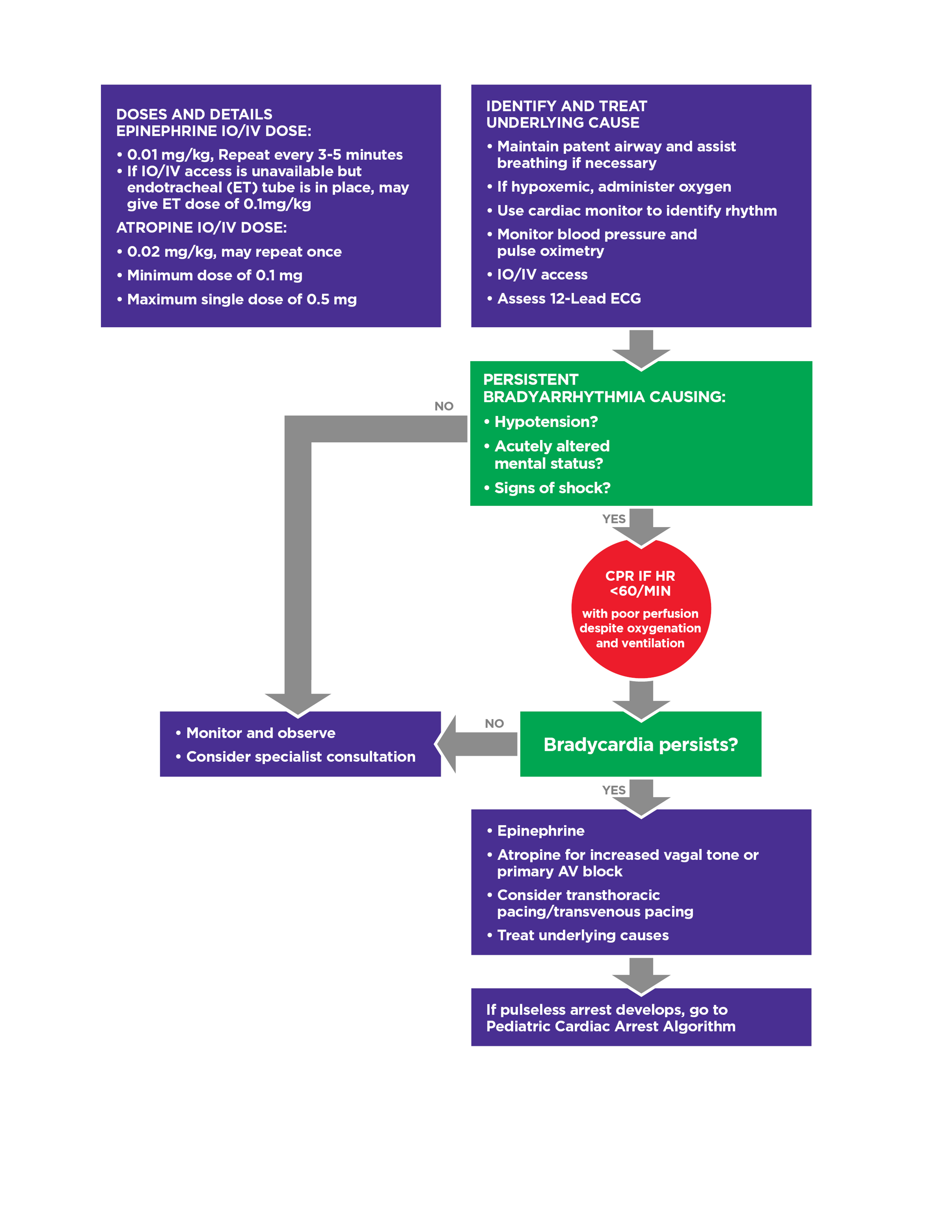
Figure 13
Key Considerations in the PALS Bradycardia Algorithm
1. Assess and Support ABCs
- Airway: Ensure the airway is open and clear; position the child appropriately.
- Breathing: Provide oxygen and support ventilation if necessary; monitor for adequate chest rise.
- Circulation: Check heart rate, pulse quality, skin color, and capillary refill time.
2. Identify Bradycardia
- Definition: A heart rate of less than 60 beats per minute in infants and children, especially when associated with poor perfusion.
- Clinical Signs: Weak pulses, hypotension, altered mental status, and signs of shock, such as pale or cool skin.
3. Evaluate for Underlying Causes
- Hypoxia: The most common cause of bradycardia in children; ensure adequate oxygenation.
- Other Causes: Consider hypothermia, acidosis, electrolyte imbalances, toxins, or increased intracranial pressure.
4. Initial Interventions
- Oxygen Administration: Provide high-flow oxygen to improve oxygen saturation.
- Ventilatory Support: Assist with bag-mask ventilation if the child is not breathing adequately.
- Monitor Vital Signs: Continuously observe heart rate, respiratory rate, and oxygen saturation.
5. Advanced Interventions
- Epinephrine: If bradycardia persists, administer 0.01 mg/kg of epinephrine intravenously or intraosseously every 3-5 minutes.
- Atropine: Consider 0.02 mg/kg of atropine for bradycardia due to increased vagal tone or primary atrioventricular block.
- Transcutaneous Pacing: If medication is ineffective and bradycardia persists, initiate pacing as per protocol.
