Shockable Vs Non-Shockable Rhythms: The Simple Guide You Looked for
Knowing which heart rhythms are shockable and which are not during an emergency cardiac event can drastically impact your chance of saving a life. As a first responder, this understanding guides your response and allows you to confidently apply what you’ve learned in Advanced Cardiac Life Support (ACLS) training.
What rhythms are shockable? What causes shockable vs non-shockable rhythms? Can you stop non-shockable cardiac arrest rhythms from occurring? I share it all in this article.
Get to Know the Cardiac Rhythms
An intricate electrical system controls your heartbeat. This network of collaborating nerves, nodes, neurotransmitters, and muscles ensures your heart beats regularly so you can pump blood efficiently around the body.
Understanding the complexity of this system is critical for the first responder. As you already know, there is no one way to save a life.  Instead, ACLS protocols are more like a tree with branches. You choose to take a branch by asking certain questions about the person’s condition and using your advanced life support knowledge to proceed confidently.
Instead, ACLS protocols are more like a tree with branches. You choose to take a branch by asking certain questions about the person’s condition and using your advanced life support knowledge to proceed confidently.
As part of these decision trees, you need to ask yourself if you’re dealing with shockable rhythms before you choose to deliver defibrillation.
What is a Non-Shockable vs Shockable Heart Rhythm?
A shockable rhythm occurs when the heart’s rhythm experiences chaos. This disruption temporarily causes it to lose its ability to properly fill the right atrium. An outside stimulus—a shock—can often correct this irregularity.
On the other hand, you have non-shockable rhythms. These types of rhythms may show no activity. They’re pulseless. But they can also be irregular, so identifying non-shockable rhythms is not as simple as checking for a pulse.
Why Do Shockable Rhythms Vs. Non-Shockable Matter?
An 8-year study performed at a hospital in Taiwan found that patients who experience in-hospital cardiac arrest (IHCA) are twice as likely to survive discharge as those who initially have non-shockable rhythms. But as a first responder, you need to realize the rhythm isn’t initially shockable as much as 87% of the time.
If a rhythm is shockable, a defibrillator can save a life by restoring a normal heartbeat. That’s true.
But for non-shockable rhythms, the patient needs immediate and uninterrupted CPR plus the right sequence of medications and medical treatments that you may be licensed to deliver.
The brain isn’t getting any blood. CPR can temporarily deliver at least some blood to the brain, making it most crucial.
That said, it’s important to realize that studies show that CPR can produce only 20% of normal blood volume (NIH.gov). If medical professionals do not restore the heart rhythm within two minutes, patients will likely suffer from some brain damage, which may be irreversible.
In as few as four minutes, permanent brain damage begins. If patients continue in this state for 10 minutes or more, they are unlikely to recover.
But note that this doesn’t mean a bystander should stop CPR after 10 minutes. These times are averages based on studies (MedlinePlus.gov). When people get trained in CPR and use an Automated External Defibrillator (AED), they learn to maintain the Chain of Survival until first responders—like you—arrive.
Once you determine that you’re dealing with a non-shockable heart, you won’t waste precious time shocking someone when another action is more likely to save their life.
What are Shockable Rhythms?
Ventricular Fibrillation (VF or VFIB) 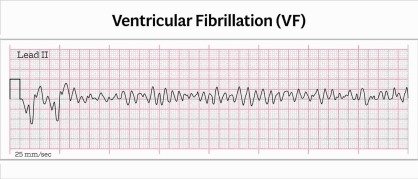
VF shows up as a chaotic, disorganized activity on an ECG (Electrocardiogram). If you have advanced your career to a paramedic, you are trained to set up and use an ECG to determine this when assessing the patient.
Pulseless Ventricular Tachycardia (VT or VTach)
These shockable heart rhythms have a regular but rapid heartbeat. However, that heartbeat often does not sufficiently supply blood to the body so you may feel no pulse.
When comparing VTach vs VFiib, the simple rule of thumb is that with VFib, the heart beats rapidly but irregularly. With VTach, you have a regular rhythm, but the cardiovascular system doesn’t effectively get blood where it needs to go. For example, uncontrolled bleeding could divert blood away from certain body parts. It could dangerously lower blood pressure.
What Conditions Lead to Shockable Rhythms?
In most cases, shockable rhythms result from severe heart conditions. These conditions disrupt the electrical impulse over time and could include:
- Myocardial infarction
- Cardiomyopathy
- Ischaemic heart disease
- Acute coronary syndromes
Some other causes can include:
- Electrolyte imbalance
- Drug overdose
- A sudden hit to the chest
How to Treat Shockable Rhythms
As soon as you determine you have a shockable rhythm, begin defibrillation. While you wait for the defibrillator to get ready, you should continue performing high-quality CPR.
Stop CPR when it’s time to shock. Then, resume CPR while the defibrillator readies itself for another shock.
Your timely and decisive action here can save a life.
What Are the Non-Shockable Rhythms?
Now that we’ve looked at what rhythms are shockable, we’ll explore those that require other actions.
Pulseless Electrical Activity (PEA)
With a PEA rhythm, the ECG reveals electrical activity but no pulse or heartbeat.  The “or” is important here because if there were only “no pulse”, that could be a shockable rhythm, VTach (described above). It’s important to put all of the pieces together.
The “or” is important here because if there were only “no pulse”, that could be a shockable rhythm, VTach (described above). It’s important to put all of the pieces together.
If you determine that someone has PEA on ECG, your response should be CPR plus airway management and medication administration within your scope of practice. Some medications that you might prescribe here include:
- Epinephrine – Constricts the blood vessels, which can increase blood flow to the brain
- Atropine – Reduce fluid in the cardiorespiratory system and treat some forms of plant or animal-caused poisoning
Asystole Meaning
Asystole is defined by the lack of electrical activity shown on the ECG. 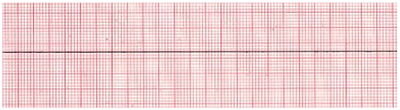 However, asystole can also include slight movement from a flatline. In fact, a complete flatline is uncommon because ventilation and chest compression efforts can make blips appear on the readout.
However, asystole can also include slight movement from a flatline. In fact, a complete flatline is uncommon because ventilation and chest compression efforts can make blips appear on the readout.
Your next steps are CPR with advanced airway management if needed, but the prognosis is poor with this one.
What Conditions Lead to Non-Shockable Rhythms?
Non-shockable rhythms most often happen in patients experiencing a serious event like:
- Massive blood loss
- Fluid buildup in the pericardial sac that compresses the heart
- Extensive heart damage
How to Prevent Non-Shockable Rhythms
The best way to prevent non-shockable rhythms happen long before you arrive on the scene and include:
- Effectively managing the underlying medical condition
- Taking medication as prescribed
- Staying well-hydrated
- Attending to lifestyle factors that can impact underlying heart conditions
But what can you do after you arrive at the emergency? You want to do what you can as a first responder to keep a shockable heart from slipping into non-shockable territory. You do this by providing immediate and effective CPR to maintain blood flow to the heart and brain. Beyond that, it’s important to follow the ACLS protocols you learned to get your ACLS certification.
A study performed by researchers at the Medical University of South Carolina found a strong correlation between following ACLS protocols to the T and return to spontaneous circulation (ROSC).
Can You Convert Non-shockable to Shockable Rhythms with ACLS?
A study published in the National Library of Medicine involved a group of researchers who reviewed data from over 40,000 out-of-hospital Cardiac Arrests (OHCA) and found that only 13% were initially shockable. That’s a very low percentage, given that patients with non-shockable rhythms cannot be resuscitated.
For this reason, in many cases, your goal as a first responder is to convert the non-shockable into ECG rhythms you can shock.
The researchers in the above studies cite their findings as showing that “Initial shockable rhythm was the strongest predictor for survival. However, conversion to subsequent shockable rhythm significantly improved post-arrest survival and neurological outcomes.”
Converting rhythms involves treating the underlying medical emergency. For example, in the case of PEA rhythm, the paramedic or EMT-IV/EMT-A on your team—which may be you—might administer Atropine intravenously to reduce the fluid in the cardiorespiratory system.
Doing so could allow the heart to start working again. But the heartbeat may still be erratic due to the VFib (a shockable rhythm). Administering defibrillation at this point could restore the heart’s rhythm. You’ve just converted the heart rhythm from non-shockable to shockable rhythm and potentially saved a life.
What Are the Types of Defibrillators?
Several types of defibrillators exist. For some, you must be a doctor or paramedic. But others, an everyday hero or the EMT-B, can use one with a current CPR and AED certification.
Manual Defibrillators
These are the ones you see in emergency room dramas or in an ambulance. Both doctors and paramedics have the skills and scope of practice to use this device. It requires rhythm analysis via ECG and manual shock delivery.
AEDs
These are the automated devices found in public spaces, such as gyms, schools, office buildings, or restaurants. They are also vital pieces of equipment for mobile first responders. The design of an AED allows those with less training to use it.
These devices analyze the heart rhythm via electrodes that you stick on the body in precise locations. They identify the right moment to administer the shock, alert you, and then deliver the shock.
The AED works like an ECG without the complicated readouts. It knows what rhythms are shockable, and it will not shock a person until that rhythm is shockable. However, AEDs cannot replace ECG plus manual defibrillators because these advanced devices give paramedics and doctors more control over when and how they administer shock. And that can make a difference.
If you’re an EMT-B, you had to learn to use AED and save a life in a CPR, AED, and First Aid Course and need to maintain your certification to renew your license every two years. If you are a police officer, firefighter or other first responder, you should also learn to use an AED.
Implantable Cardioverter-Defibrillators (ICD)
A doctor can prescribe this long-term management device to help regulate a rapid heart rate if you have a history of cardiac arrest. It automatically detects and treats ventricular arrhythmias. Unlike pacemakers, which regulate the heart from the top, an ICD regulates the lower heart (ventricles).
Use Your Advanced Cardiac Life Support (ACLS) Training to Save Lives
ACLS Algorithms 
You can find all of the concepts we’ve discussed laid out visually and sequentially in your ACLS algorithms for cardiac arrest. This tool walks you through a decision tree to determine shockable vs non-shockable rhythms and what steps to take.
As a lifesaving professional, you must familiarize yourself with these algorithms in advance. Time is of the essence. Even if some of this is outside of your scope of practice, you may assist paramedics or doctors following this protocol. Learning ACLS allows you to effectively coordinate efforts to save a life.
The algorithm begins with three quick steps:
- Start CPR
- Give Oxygen
- Attach heart rhythm monitoring device (i.e., ECG)
Next, you must ask if the rhythm you see on the ECG is shockable.
If it is PTV or VF, then yes. If PEA or Asystole, then no.
Follow the appropriate branch.
For shockable, delivering defibrillation is the next step. After that, perform CPR for two minutes and prepare IV/IO access.
Again, ask yourself if the rhythm is shockable. If the answer is no, you’ll jump over the non-shockable branch of the algorithm and begin administering epinephrine via that IV access you created.
But if the rhythm is still shockable, you will shock first and then start the epinephrine. Continue CPR for two minutes. At this stage, you might consider advanced airway management or capnography to measure CO₂ exhalation.
If the rhythm continues to be shockable, you will deliver shock again and then administer Amiodarone or Lidocaine. Treat any reversible causes. Here, you use your professional judgment to give the right medications based on the patient’s symptoms.
And repeat the process.
On the non-shockable side, you are performing the same steps without the shock as you attempt to convert the non-shockable to shockable rhythms with ACLS.
To get a more thorough, visual, and easy-to-follow representation of these decisions, why not print the ACLS Cardiac Arrest Algorithm or save it on your phone?
This algorithm is based on the evidence-based best practices established by the International Liaison Committee on Resuscitation.
Shockable Vs Non-Shockable Rhythms
When split seconds matter, knowing what rhythms are shockable allows you to take the most appropriate steps to save a life confidently. But distinguishing shockable vs non-shockable rhythms isn’t as easy as checking for a pulse. You’ll need an ECG if you’re a medical professional. For everyday lifesaving heroes, learning how to use AED is the second best.
As a first responder, learning CPR and ACLS allows you to take an evidence-based course of action whether you are performing advanced medical procedures or supporting someone who is. Learn more about becoming ACLS certified here.

