Cardioversion vs Defibrillation: What’s the Difference?
Cardioversion vs Defibrillation: What's the Difference?

by Greta Kviklyte
Life Saver, AMC
Co-authored by Kim Murray, RN, M.S.
posted on Aug 26, 2021, at 8:30 am
Cardioversion vs defibrillation are two potentially life-saving methods that are critical for all rescuers to understand. If you are facing the need to provide synchronized cardioversion vs defibrillation or how to treat an irregular heart rate, read on.
Each year, an estimated 300,000 cardiac arrests happen in U.S. hospitals, of which some 81% are non shockable rhythms (asystole or pulseless electrical activity). In 50-60% of cases, cardiac arrest happened because of primary heart failure, followed by primary respiratory failure at somewhere over 15%. This is according to a JAMA study published at NIH.gov.
The only proven rhythm method to improve the survival rate to discharge is timely defibrillation after a cardiac arrest, secondary to ventricular tachyarrhythmia.
We offer Online CPR and BLS Certification
However, for certain types of cardiac arrhythmias, the most effective treatment is synchronized cardioversion. So it’s important to know the difference between cardioversion and defibrillation, when they’re used, and when one or the other may be dangerous and even cause cardiac arrest.
Synchronized Cardioversion Vs. Defibrillation: Overview
The goal of both defibrillation and cardioversion is to transfer electrical energy to the heart. This stuns the heart instantly in hopes of generating a normal sinus rhythm from the heart’s natural pacemaker, which the heart can then maintain on its own.

While both use the same general action and can use the same equipment, the method is different, as well as when you use them, how you use them, and why you’re shocking the heart.
Primarily, you use defibrillation during an immediate life-threatening situation. You have a cardiac arrest, and if you don’t get this heart restarted, the victim will officially transition.
Conversely, doctors use cardioversion to convert heart rhythm when a patient has an unstable heart but is not immediately in danger of dying. Cardioversion stabilizes the heart rhythm. It is, therefore, usually an elective procedure. With guidance from their doctor, a patient chooses cardioversion to correct their heart rhythm. But it can also be urgent if the patient is experiencing tachycardia or a feeling of breathlessness.
Second, doctors synchronize cardioversion to achieve a specific rhythm outcome. You don’t time defibrillation. You just need a shockable rhythm.
So, as soon as there is a shockable rhythm, an automatic defibrillator tells you to “hands off” or “clear”. Then a shock occurs. But during cardioversion, the machine waits a couple of seconds to sync up with the rhythm to shock at a precise time in that rhythm.
Third, a defibrillator delivers a higher energy dose vs. cardioversion.
Ultimately, cardioversion performed when needed could prevent a subsequent cardiac arrest later that day, week, or year. That’s because it transforms an irregular rhythm into a stable one. But once a cardiac arrest occurs, defibrillation is your only option–that is, if you have a shockable rhythm.
Below you’ll find further information about these procedures to further distinguish between them.
Cardioversion vs Defibrillation: A Chart for Easy Comparison
Use the following chart to help you see the differences between cardioversion and defibrillation. Then, read on about the process of providing care.
Defibrillation vs Cardioversion |
||
| Category | Defibrillation | Cardioversion |
| Patient Condition | The patient is in cardiac arrest or has no heartbeat | The patient is functional but has an irregular heartbeat |
| Energy Levels | Between 150 and 360 joules | Between 50 and 300 joules |
| Synchronization | Is done as necessary | Set to a specific point according to an EKG |
| Sedation Requirement | Midazolam or Diazepam | Midazolam or Diazepam |
| Typical Arrhythmias Treated | Life-threatening arrhythmia | Used to convert an arrhythmia back to sinus rhythm, such as with atrial fibrillation |
What Is Defibrillation?
Defibrillation is a shock-based treatment for life-threatening arrhythmias when a patient does not have a pulse. These could include ventricular fibrillation (VF) or pulseless ventricular tachycardia (VT). It’s done when someone is in cardiac arrest.
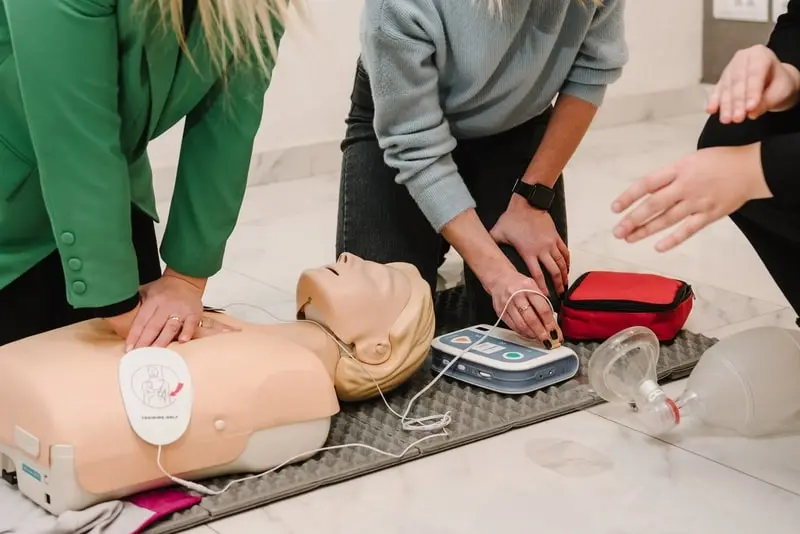
Someone can perform it in a hospital, an ambulance, or an out-of-hospital setting. While medical professionals perform defibrillation in the hospital, the average person with CPR training can also perform defibrillation if they have access to an automatic external defibrillator (AED). You can buy one for your home or office.
A Brief History of the Defibrillator
Two physiologists (Prévost and Batelli) discovered the power of fibrillation around the end of the 18th Century by running dog experiments using shock. They found that when they applied small shocks to the dog’s heart, they could put the heart into V-fib and then shock it again with a larger shock to reverse the change.
But it would be another 14 years before a cardiothoracic surgeon did defibrillation on a 14-year-old boy on whom he was performing cardiothoracic surgery for a congenital heart disorder. He placed electrodes on the open heart for the procedure.
The technology remained mostly unchanged for another 150+ years until the 1950s, when Russian researchers developed a defibrillator that they could use on a closed chest. This would later become the modern-day monophasic defibrillator. In the 1980s, researchers discovered a biphasic waveform, which would replace monophasic shocks in some instances.
Defibrillation and Cardioversion share this history since they both use a defibrillator to work.
Monophasic Vs. Biphasic Shock
A monophasic shock only travels in one direction from one paddle to another, while a biphasic shock travels from one paddle to the other and then back several times. Biphasic shock results in fewer burns and has a higher first shock success rate (90% to 60%), although studies comparing how use may impact discharge success haven’t been thoroughly studied.
Types of Defibrillators
There are four primary types of defibrillators, which are used in different settings:
- Automated External Defibrillators (AEDs) are often found in CPR kits for the average person with CPR training.
- Semi-automated AEDs can be overridden and are therefore only used by a trained professional like a paramedic.
- Standard defibrillators with monitors require professional skills to operate. You’ll find them in hospitals mostly.
- Implanted defibrillators can shock the heart back into a rhythm during a cardiac arrest without assistance from a bystander.
While paddles were once very common, they’ve now been overtaken by the use of adhesive patches, which are generally easier to use and perform better because they adhere to the chest without the need for gel application.
Risks of Defibrillation
Defibrillation risks are minimal when the machine is well-maintained. Defibrillators measure the patient’s heart rhythm and, if you have an automatic machine, they provide clear instructions based upon that rhythm. All you have to do is follow his instructions even if you have no medical training.
Fragile patients, like the elderly, may experience broken ribs or the aggravation of an existing injury. But defibrillation saves a life, so those are generally considered reasonable casualties of the procedure.
Shocking yourself is also possible, so when the machine says “hands off”, please make sure no one’s touching the victim.
Defibrillator burns have been reported but are rare with current equipment and a sign of a poorly-maintained machine that probably needs to be replaced. The batteries and pads of an automatic defibrillator typically last two to five years, depending on the frequency of use. So they need to be replaced to maintain proper function. An implanted defibrillator lasts up to 10 years, according to Johns Hopkins at HopkinsMedicine.org.
These same risks will apply to cardioversion plus a few more.
Energy Levels for Defibrillation
- Monophasic – CPR algorithm recommends single shocks started at and repeated at 360 Joules (J).
- Biphasic – CPR algorithm recommends shocks initially of 150-200 J. Then use subsequent shocks incrementally 150, 200, 300, 360 J.
A clinical trial on biphasic defibrillation showed that increasing the energy level of shocks was more likely to result in a conversion and stop ventricular fibrillation (VF) when compared with repeated shocks at 150 J. Often, the first shock did nothing, but the subsequent higher J shock did.
What Is Cardioversion?
 Synchronized cardioversion is a process to achieve a sinus rhythm in a patient who has arrhythmia. It requires the delivery of a low energy shock at a specific time. Doctors achieve this timing by viewing a defibrillator monitor or using a machine that syncs to the rhythm automatically. In both cases, you’ll only find this equipment in a hospital or specialized clinic.
Synchronized cardioversion is a process to achieve a sinus rhythm in a patient who has arrhythmia. It requires the delivery of a low energy shock at a specific time. Doctors achieve this timing by viewing a defibrillator monitor or using a machine that syncs to the rhythm automatically. In both cases, you’ll only find this equipment in a hospital or specialized clinic.
They sync the shock to a specific point in the QRS complex (the main spike visible on that monitor with EKG / ECG).
Through this method, atrial fibrillation can be converted to a normal sinus rhythm while preventing the prompting of ventricular fibrillation (VF). This happens because you’ve synchronized the electrical shock to the R wave. At the same time, you avoided that susceptible T-wave and averted ventricular fibrillation.
Uses & Indications
Patients who need cardioversion experience the following symptoms:
- Breathing struggles from pulmonary edema (fluid in the lungs)
- Hypotension (low blood pressure)
- Chest pain
- Syncope (loss of consciousness from low blood pressure)
When a patient has symptoms like these, their doctor will need to run tests to confirm the cause of the symptoms.
Electrical cardioversion may be indicated if those tests show:
- Unstable pulse
- Failed chemical cardioversion with chest pain or unlikelihood chemical cardioversion would be successful.
- Decompensated rapid AF with rapid ventricular response. An example of this would be a hypotensive patient who isn’t responding to other medical therapies.
- Ventricular tachycardias (VT) with pulse
- Supraventricular tachycardias, which includes AF without decompensation but only if not in an acutely urgent situation.
The technique is used less frequently in situations such as atrial fibrillation to revert the heart rhythm to a sinus rhythm.
In a patient with atrial fibrillation, you use cardioversion to control the rhythm. However, cardioversion will not always be successful. Studies have shown as many as 50% of patients’ hearts will return atrial fibrillation within 12 months. However, a doctor could do another cardioversion at that time, if needed.
Risks of Cardioversion
In addition to the general risks of defibrillation, you should stay aware of these potential complications.
Having cardioversion may put patients at increased risk of thromboembolic disease (TED) soon after the procedure. As a precaution, doctors prescribe anti-coagulation at least three weeks before and four weeks after the procedure.
Doctors may also use a transesophageal echocardiogram during the procedure to spot thrombus, although some patients may still develop TED.
How to Cardiovert
 Cardioversion is performed in a hospital with a doctor, an anesthesiologist, and cardiac nursing professionals present. The anesthesiologist will plan and supervise sedation of the patient using general anesthesia. Once sedated, the team performs the following steps:
Cardioversion is performed in a hospital with a doctor, an anesthesiologist, and cardiac nursing professionals present. The anesthesiologist will plan and supervise sedation of the patient using general anesthesia. Once sedated, the team performs the following steps:
- Attach the self-adhering electrodes
- Pick an energy level to start. Note: a higher starting energy may require fewer shocks. Levels are based on the starting type of rhythm. For Broad complex tachycardia and AF, you’d do monophasic starting at 200 or biphasic at 120-150 J. For atrial flutter and narrow complex tachycardia, the recommendation is starting at 100 for monophasic and 70-120 J for biphasic
- Achieve a visible trace on the monitor
- Hit the sync button. You’ll see a blip or dot marking the QRS complex. This will allow the shock to sync automatically so it shocks with correct timing that might not be achieved manually. Note: sync may not work in tachycardia where the QRS complex is variable.
- Charge
- Call “Clear” and look to see that the bed is clear.
- Shock. Expect a 1-2 second delay since the machine is synchronizing the shock.
- View the rhythm to see if you have a sinus rhythm. If yes, stop. If not, adjust the energy level up incrementally and repeat steps 5-8.
- Look for burns that may need treatment
- Get a 12-lead ECG for a more thorough reading
Special Considerations on Infants and Children
Pediatric Cardioversion and Defibrillation require attention to detail and some basic math skills. The recommendation is to start at 1J for every kilogram of weight.
You should never use an automatic or semi-automatic defibrillator on a child younger than one year. Only use a manual one with a monitor, which usually means the child is in the hospital.
Whether performing on an infant or child, note that manual defibrillators only go as low as 4J/Kg, so use specialized pediatric pads for both manual and automatic external defibrillators. This reduces the energy delivered when used in combination with the pediatric setting. You can view further details related to pediatric treatment in Pediatric Cardiac Arrest Algorithm.
Children eight and older can receive cardioversion and defibrillation at adult levels, according to the guidelines outlined in your Advanced Cardiac Life Support Training. You can now obtain this training 100% online.
Pediatric defibrillation is complex in that the recommended shock level is much lower, beginning with a dose of 2 J/kg and use of 4 J/kg for subsequent attempts. Because ventricular fibrillation occurs in 8 to 20% of pediatric cardiac arrests, it is critical to consider the best treatment possible when administering this shock. Data indicates that, with every 1 minute of delay in defibrillation, the survival rate of the child falls by 7 to 10%.
Cardioversion Vs. Defibrillation
Cardioversion and defibrillation both rely on the power of shock to achieve the desired heart rhythm. But when they’re needed and how doctors use the defibrillation equipment are very different. Exploring the differences between procedures with so many similarities can help you better understand how the heart works and how doctors can apply different strategies to help the heart perform at its best.
Chemical vs Electrical Cardioversion
In the comparison of cardioversion vs defibrillation, consider the mechanisms used. Studies indicate that chemical vs electrical cardioversion can be a critical factor for doctors and rescuers to consider, and no single consensus exists on which method is the preferred option.
In short, a chemical cardioversion occurs when an abnormal heartbeat is cardioverted to a normal rhythm using medications. These medications work to get the heart back into normal rhythm. By comparison, electrical cardioversions use electrical shock to adjust the rhythm of the heart.
Both methods may be effective, and electrical cardioversion may be faster at converting a person. For those who cannot be shocked, the use of medication may be necessary.
Note that in cardioversion vs defibrillation, only cardioversion allows for a true chemical treatment. Defibrillation only occurs with the application of electrical energy, though both methods may be used during this process.
Synchronized Cardioversion vs Defibrillation
 You may hear a significant amount about synchronized cardioversion vs defibrillation or defibrillation vs synchronized cardioversion. Let’s break down some of the core elements of this comparison of cardioversion vs defibrillation:
You may hear a significant amount about synchronized cardioversion vs defibrillation or defibrillation vs synchronized cardioversion. Let’s break down some of the core elements of this comparison of cardioversion vs defibrillation:
- Synchronized cardioversion: This process occurs in a specific part of the heart’s beat cycle. More precisely, the first step is to recognize the electrical impulses that control the heartbeat and then measure them accurately. This allows for a jolt to be administered at a very specific time within the heart’s beating cycle, which could improve cardioversion outcomes. These cardioversions are timed.
- Unsynchronized cardioversion: These cardioversions require the use of more energy because they are untimed and, therefore, can deliver a shock at any time during the cardiac cycle. This type of cardioversion is much more in line with a defibrillator.
In many cases, an unsynchronized cardioversion is the same application and treatment process as a defibrillation. It occurs at any time after the machine charges and is ready to fire, even without any monitoring of the heart’s beat.
How to Cardiovert in the Field
Cardioversions happen in a hospital setting. However, if there is an AED available, rescuers can use it with proper education. Rescuers can learn how to cardiovert using an AED after taking a licensing exam. From the objective of the patient, the process will include:
- Being under twilight sedation
- A cardioverter machine will deliver a quick jolt of energy to the patient. This energy, delivered to the heart through the placement of cardioversion pads, changes the beat.
- It interrupts the abnormal beat or electrical rhythm of the heart and then restores normal heart rhythm, which is more natural and what the heart wants to beat.
In some situations, it may take several shocks to restore the normal function of the heart. The procedure only takes a few minutes. If you are a rescuer and wish to learn how to administer a cardioversion or defibrillation in an emergency, complete the CPR, AED & First Aid Certification Course we offer.
What is atrial fibrillation?
Atrial fibrillation is often a component of cardioversion vs defibrillation conversations. It indicates the heart’s quivering action or irregular heartbeat in the atrium or the upper chamber of the heart. Often called Afib, this condition is not usually life-threatening, though it can prolong complications to the heart and lead to complications over time.
Which is better, unsynchronized cardioversion vs defibrillation?
An unsynchronized cardioversion is the same as defibrillation. These types of cardioversion do not have a timed or planned moment of transferring the energy to the other patient. Rather, as soon as the device is charged up, it is applied without paying attention to the actual cardiac cycle.
What are synchronized cardioversion joules?
Synchronized electrical cardioversions typically utilize a recommended energy level of 50 to 300 joules, depending on the person’s age and overall condition. A narrow regular level indicates joules of 50 to 100 joules. If a wide regular heartbeat occurs, 100 joules are used. With a narrow irregular rate, 120 to 200 joules are used. What is the difference between synchronized and unsynchronized cardioversion? Synchronization indicates that the jolt of energy is applied at a very specific point in the cardiac cycle or the process of each heartbeat. This can help to change the heart rate back to normal rhythm without the use of as much electrical shock as what occurs in untyrannized cardioversions.
Ready to Learn More?
Enroll in the ACLS certification course now. Doing so allows you to learn more about cardioversion vs defibrillation and teaches you how to take action during an emergency medical event.





 A defibrillator program is only one aspect of preparing your business for an emergency. However, before you decide to install a program and begin the process of ensuring its success, you should get
A defibrillator program is only one aspect of preparing your business for an emergency. However, before you decide to install a program and begin the process of ensuring its success, you should get