ACLS Algorithms and Epi-Administration: An In-Depth Review
The International Liaison Committee on Resuscitation (ILCOR) published an updated list of ACLS algorithm guidelines every five years. The updated list reflects the latest research and evidence-based practices to enhance survival and life expectancy following cardiac or pulmonary arrest. The most recent rendition of guidelines did not involve a change to epinephrine, also known as adrenaline, administration.
Epinephrine is the preferred medication in encouraging a return of spontaneous circulation (ROSC). The fight-or-flight hormone has immense effects on the body, increasing chances of survival.
As a result, some organizations and health care facilities have grown accustomed to the use of epinephrine as the essential step in reducing cardiac arrest mortality. Sadly, this includes the early administration of epinephrine, even when it is not necessarily indicative of the current algorithm.
A recent study on the efficacy of early administration of epinephrine reveals a much bigger problem. Too much may lead to worsening of health and increased mortality risk. Health care professionals need to know what the study means for ACLS response and how to prevent over‐medication that may result in higher risk of death.
The Debate Over Epinephrine Administration in the ACLS Algorithm
Epinephrine is indicated for its vasoconstriction effects in the body, increasing blood pressure to ensure proper profusion of oxygen and nutrients. It also enhances cardiac output by increasing the heart rate, contractility, and conductivity within the AV node. These factors have led multiple EMS departments, whole hospitals, and acute‐care facilities to wholeheartedly embrace the administration of epinephrine regardless of time. However, the Journal of Emergency Medical Services (JEMS) recently reviewed a study finding significant setbacks to health outcomes as a result of poor administration of epinephrine.
Much debate exists over when and why epinephrine should be administered in cardiac arrest. Variances exist for weight, age, and cause of cardiac arrest. Anaphylaxis, shock, and chronic health conditions may lead to cardiac arrest in any setting, including in‐hospital and out‐of‐hospital environments.
Studies Suggest Early Epi‐Administration Offers Little to No Benefit
Delivery time of epinephrine in patients determines survivability and long‐term health outcomes. Current ACLS protocol dictates the administration of epinephrine after the second round of defibrillation. This means a non‐shockable rhythm should never involve the administration of epinephrine before the initial shock, yet many hospitals and EMS systems administer epinephrine earlier than recommended. Such a common practice warranted additional research.
A study of the early administration of epinephrine found little to no benefit to those in cardiac arrest. While administration of epinephrine was believed to have an increased chance of ROSC, study participants that received early administration prior to the second shock had a decreased rate of ROSC. Approximately 12-percent fewer people had a ROSC due to early administration, and up to 17 percent of those that received early dosing lost their lives.
The study also sought to eliminate confounding factors, so all patients studied were matched in terms of age and underlying diseases.
Effect of Epinephrine in Cardiac Arrest
Understanding the relationship between ROSC, epinephrine, and poor outcomes requires comprehension of how epinephrine acts on the body and cardiovascular system.
As explained by the National Library of Medicine, epinephrine stimulates α1 receptors in vascular smooth muscle. Vascular smooth muscle contracts in response, increasing perfusion pressure and encouraging a return of spontaneous circulation (ROSC). However, coronary circulation is effectively reduced. As high plasma levels of epinephrine continue to act on the body, additional arrhythmias may occur, including life‐threatening ventricular fibrillation.
Resulting arrhythmias arise from high plasma concentrations after ROSC, so creating an excessive concentration too early may increase the risk of subsequent cardiac arrest. This is the great paradox of ACLS administration. Epinephrine is necessary in the process, but it also can be a cause of cardiac arrest. The cycle continues until equilibrium is achieved, and since long‐term hospital stays are generally associated with poorer outcomes, life‐expectancy and quality decrease further.
ILCOR Recommendations for Epinephrine Aren’t Necessarily Applied Properly
A significant cause of concern in the study rests on the differences between facilities and practitioners providing ACLS. Depending on the responding party, as well as the setting, administration of epinephrine may vary widely.
EMTs may follow county‐specific guidelines for ACLS, even when such guidelines are contradicted by existing ILCOR recommendations. An astounding 50 percent of cardiac arrest patients in the JEMS study with a shockable rhythm received early dosage of epinephrine. That’s not all.
Early administration of epinephrine also differs by age group. Some areas may follow an algorithm advising early administration of epinephrine in children suffering traumatic, out‐of‐hospital cardiac arrest.
While this may be suitable for children experiencing hypovolemic shock, the adverse effects still exist. Moreover, the metabolism of children and a lack of study on the long‐term effects of early epinephrine administration in children further constrains treatment measures after ROSC. A 2016 study on the administration of epinephrine in children following traumatic cardiac arrest supports the argument against early administration, asserts NCBI.NLM.NIH.GOV.
In the adult JEMS study, survival chances decrease; cognitive function may be further impaired; and recurrence of cardiac arrest becomes more likely. The study of children found similar poor outcomes. However, the study also notes that the nature of trauma may contribute to such outcomes. Isolating the information within the child study does reveal one key point; early administration of epinephrine does not increase chances of survival or better neurologic outcomes among children.
Fast-Paced Survey of Health Care Facilities in Texas Indicates Widespread Disagreement
Although up to 50 percent of patients in the JEMS study received early administration, actual rates of early administration can vary as high as 60 percent. Keep that number in mind.
As part of the thorough review of available resources in writing this article, a survey of Texas panhandle health care facilities was conducted. The survey included health care facilities across the region, comprised of hospitals, EMS systems, emergency departments, and long‐term acute care facilities. The survey consisted of requesting information regarding facility‐specific ACLS guidelines in administering epinephrine. It is important to note that only 11 different EMS systems were part of this survey. This is due to the nature of multi‐county, integrated EMS systems.
The survey found the prevalence of earlier‐than‐recommended dosing of epinephrine in cardiac arrest is rampant, beyond the rates noted by JEMS. After contacting each facility, the survey focused on asking three key questions relating to cardiac arrest and epinephrine administration.
Out of 84 responding hospitals, 20 were incapable of responding to questions one and three, shown below.
1. Do staff administer epinephrine within the first two minutes of cardiac arrest?
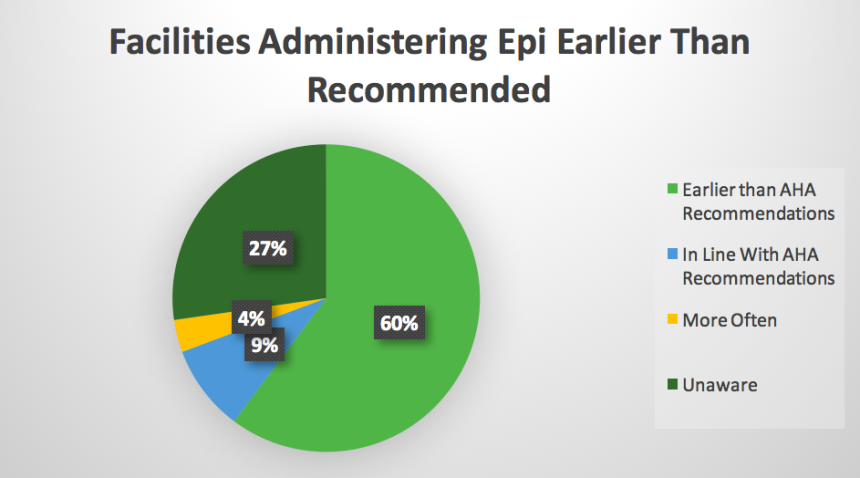
This graphic details the earlier administration of epinephrine than the ILCOR recommend, facilities administering the medication after the first shock and those administering epinephrine more often than advised. In other words, 4 percent of responses included the administration of epinephrine at the lowest end of the interval, if not occurring up to 30 seconds faster than advised.
Given the current recommendation of 1 mg every 3–5 minutes, actual dosage over a 10-minute span could be as high as 3 mg. Paired with factors like BMI and underlying health conditions, recovery from the effects of epinephrine administration due to plasma levels could lead to poor treatment outcomes and even death.
2. How often have epinephrine administration guidelines for the facility changed?
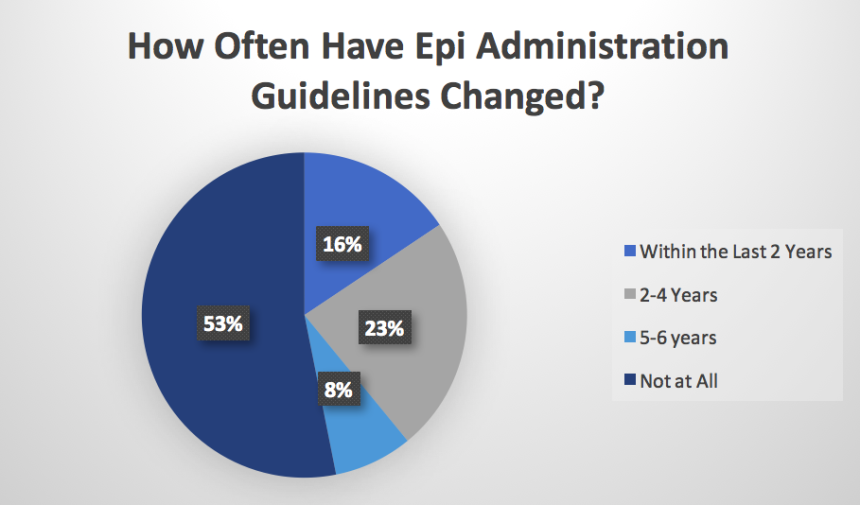
This question was an attempt to define the current understanding of ACLS recommendations from 2015. Although the guidelines regarding epinephrine did not officially change, they did include a mention of the potential setbacks from early administration. Moreover, those completing ACLS for a subsequent certification period may have not yet been exposed to this material. In other words, it is not necessarily uncommon to see changes advised in recent years.
Since only 16 percent were able to recount the need to avoid early administration, this effectively means up to 86 percent may believe county‐ or facility‐specific guidelines are superior to ILCOR recommendations. The only way to change that lies in reviewing the recommendations now. For instance, someone within the 86 percent should consider completing an online ACLS certification course, even if the existing certification is still valid.
More importantly, the prevalence of this assumption should warrant the retaking of all ACLS courses in all facilities to further reduce risk of early administration of epinephrine.
3. If guidelines have not changed, were supervisors or nurse educators aware of new recommendations to avoid early dosing of epinephrine, before administering shocks?
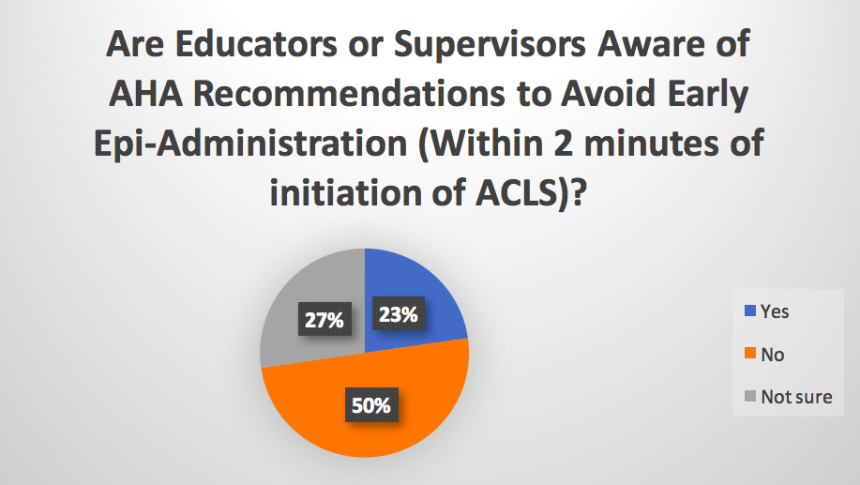
The final question builds on the second. Instead of focusing on the facility‐wide protocols, the survey drilled down into the individuals responsible for making decisions regarding ACLS certification and facility‐specific protocols—nurse educators and supervisors.
The results of this question are more worrisome. While 50 percent of respondents indicated they were not aware of the ILCOR recommendation to avoid early administration of epinephrine, 27 percent were simply not sure.
This is the confusing part of this study due to the leading nature of the question. Some may have answered in accordance with the question’s implication. In other words, more may have answered “Yes” or “Not sure” as a means to avoid answering “No.” Even so, only 23 percent were able to say definitively that they knew about the recommendation.
Long‐term survival rates of early administration of epinephrine are less than 1 percent. In Texas, 22.5 percent of deaths are related to cardiovascular problems, reports DSHS.Texas.Gov. Excluding cardiac arrest caused by non‐cardiovascular diseases, like anaphylaxis or accident, ensuring an average survival rate with proper dosing can have a tremendous effect.
Applying the Survey to a Potential Change in Mortality Rates
While not all cases of cardiac arrest result in ROSC, a significant number of lives may be saved by simply increasing awareness of appropriate dosing timelines. Based on the information within the survey, up to 77 percent of cardiac arrests resulting in death could have a link to the early administration of epinephrine; although, additional studies would be necessary to clearly define survival rates.
Using data regarding average, national survival of cardiac arrest and Texas mortality rates, another insight becomes evident. According to the ILCOR, the national average rate of survival for cardiac arrest is 18.4 percent. This is the average of both the survival rates in‐hospital (24.8 percent) and out‐of‐hospital (12 percent) rates. If survival chances decrease to 1 percent due to early administration, the survival rate effectively decreases 17 percent.
Combining this with information from the JEMS study alludes to the possibility of eliminating this decrease in 50 percent of those that suffer cardiac arrest. Therefore, cardiac arrest mortality may have the potential to be reduced by one‐half simply through the prevention of early administration of epinephrine. In other words, average survival rates could rise to 36.8 percent. That means one in three lives could be saved, as opposed to one in five or eight, depending on in‐hospital and out‐of‐hospital settings.
Review of ACLS Guidelines and New Protocols Are Critical to Reducing Mortality
Early administration of epinephrine goes against ILCOR recommendations and diminishes the survival rate of those suffering cardiac arrest. The statistics and prevalence can be overwhelming, but they boil down to two facts. First, health care professionals need to be aware of the ILCOR recommendations, even when they are in contrast to the facility guidelines. Second, those that do know the guidelines have a duty to encourage change in their organizations.
It may simply be that those making decisions regarding ACLS algorithms and protocols have not yet encountered the research on the adverse effects of early administration of epinephrine.
Remember to sign up for your refresher course to learn more about the latest guidelines regarding epinephrine administration and ACLS today. Also, share this article on social media to help spread awareness about the problem of early administration of epinephrine that goes against ILCOR recommendations.

