Heart Anatomy and Physiology; Cardiovascular Anatomy & Physiology
An important aspect of properly performing ACLS is having a strong understanding of normal cardiac anatomy and physiology. The heart—a hollow muscle—has four chambers that are kept in place by thick walls of tissue, known as the septum. The two lower chambers are known as the ventricles, and the two upper chambers are the atria. The two halves of the heart work together, performing the main function of pumping blood around the body.
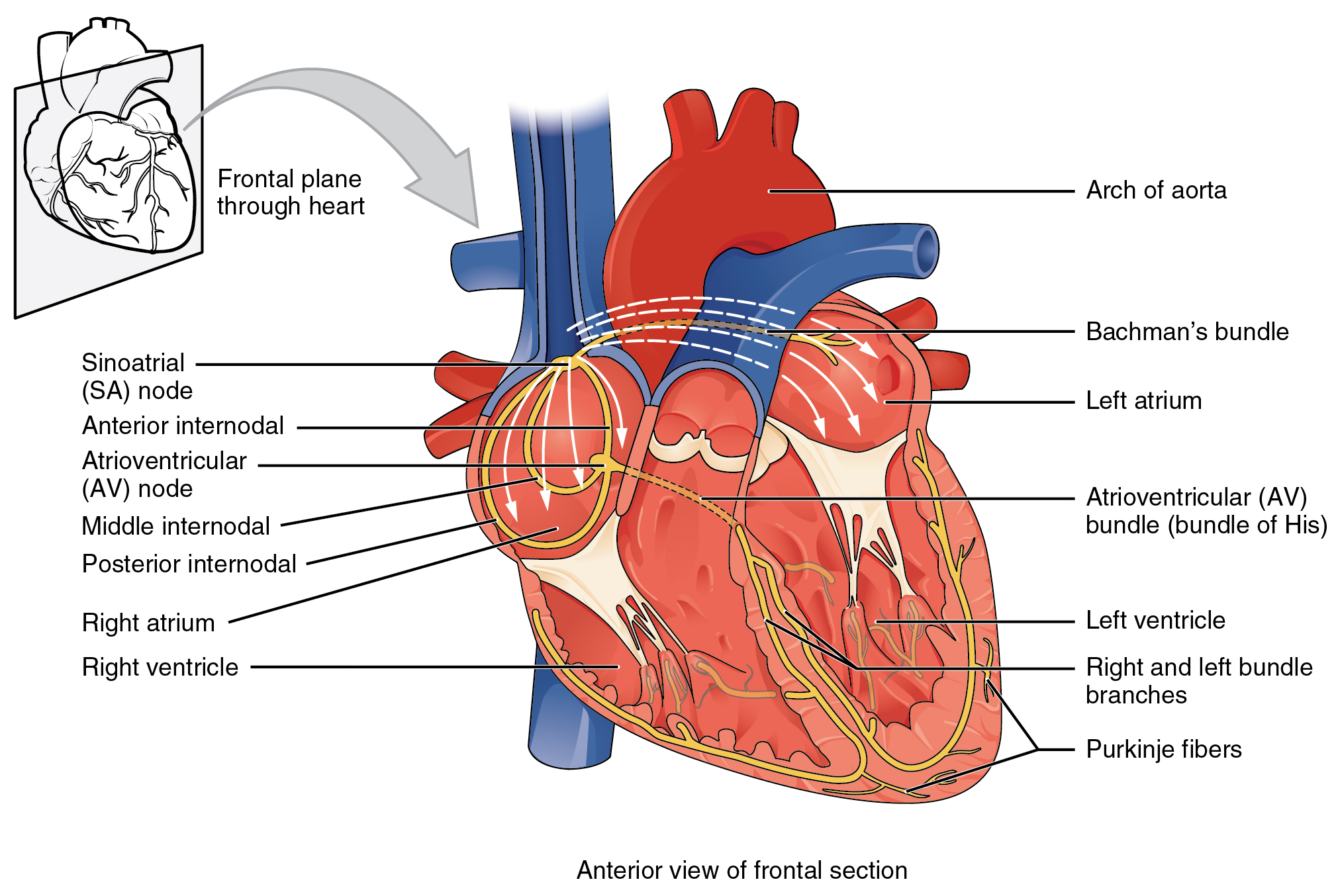
Figure 8a
Deoxygenated blood is pumped to the lungs by the right ventricle (RV) and the right atrium (RA), where it then becomes oxygenated. After becoming oxygen-rich, this blood travels back to the left atrium (LA) and enters the left ventricle (LV). The left ventricle is the main pump, delivering the enriched blood all throughout the body. The aorta, a large vessel in the heart, is where the blood exits. Between the pairs of connected chambers are valves that stop blood from flowing back.
The heart’s contractions move from top to bottom due to the simultaneous contraction of the two atria and ventricles. Each of the heart’s beats starts in the RA. The thickest-walled and biggest of the four chambers is the LV, which is the chamber that is concerned with distributing the oxygenated blood throughout the body. In the RA is what is called the sinoatrial (SA) node, which generates electrical activity that works in keeping the heart’s natural pace.
This electrical activity is then forwarded to another node known as the atrioventricular (AV) node, which rests between the ventricles and the atria(Figure 8a). It pauses there for a while before then traveling to the His–Purkinje system; this system is a sort of wiring that transfers the electrical activity into the LV and RV. The heart muscle moves, contracting, and pumping blood, due to this electrical activity.
Understanding abnormal functions are easier when you understand how electricity functions in the heart. As blood goes into the heart’s atria, an electrical impulse is generated that travels from the SA node and through the atria, which leads to the atrial contraction.
This is known as the P wave—the atrial contraction is recorded on an electrocardiogram (ECG) strip. This activity moves to the AV node, which then conducts the electrical activity through the bundle branches, the Bundle of His, and ventricles’ Purkinje fibers, resulting in contraction of the ventricles. The ECG strip registers the time between the atrial contraction and the start of the ventricular contraction as the PR interval, and this ventricular contraction is then registered as the QRS complex. The ventricles slow down, repolarizing and resting, after ventricular contraction, which the ECG strip registers as the T wave. The repolarization of the atria also occurs, although this cannot be observed on the ECG strip, as it happens simultaneously with the QRS complex. The T wave, QRS complex, and P wave come together and are indicative of an NSR (Figure 8b, found on next lesson), or normal sinus rhythm.
The transmission of electrical activities is sometimes delayed by conduction system abnormalities and defects, and this is read on the ECG. When deviations such as these occur, it can lead to dysrhythmias or heart blocks; pauses; bradycardias and tachycardias; dropped beats; and blocks. This handbook will focus on these disturbances in more detail later.
