Synchronized Cardioversion: Guide to Safely Treating Rapid Arrhythmias
Picture it: Your patient is in front of you, their heart racing uncontrollably—and yours is rising too. That beat is somewhat erratic but relatively predictable. You’ve tried medication, but nothing is working. The clock is ticking. You need to act fast. In this moment, synchronized cardioversion with its precise shock to the heart could completely turn this situation around.
As a health care professional, you often face high-stakes, life-threatening emergencies like this. Synchronized cardioversion is one tool you learn to use to save lives when time is a luxury you don’t have. Understanding this technique isn’t just about knowing how it works. It’s about knowing when to use it and how to do it safely.
In this go-to guide, I break down everything you need to know and share some ways you can test your knowledge and decision-making before you have a patient on the table. We’ll compare it to other techniques like defibrillation and discuss how to manage the risks.
Whether you’re studying for your ACLS certification exam or you want to casually learn more about this topic, this guide will give you more confidence in those critical moments.
What is Synchronized Cardioversion?
Think of the heart like an orchestra. When it’s healthy, every beat follows a steady rhythm. That pace does increase and decrease based on what the patient is doing or, in some cases, thinking. However, there’s a method to it. It’s music!
Now, sometimes, this rhythm gets out of sync. It’s up to the conductor to get everything working together again. They have to get everyone’s attention with a bold move that forces the musicians back in line with the piece they rehearsed.
This is synchronized cardioversion, a controlled electrical shock that stops arrhythmia (irregular heartbeat). This jolt halts the chaos that has ensued, giving the heart an opportunity to reset itself.
How Does Synchronized Cardioversion Work?
Here’s the science behind it: the machine, usually a defibrillator, monitors the heart rhythm to time the shock. These machines can detect the R wave (the point of contraction) and deliver the shock at that moment. This timing is critical because if the shock were not so precise, it might deliver the shock on T wave (repolarization).
The T wave represents the repolarization of the ventricles (when ions flow back in). Then, during depolarization, ions (electrolytes) flow out of the cells, initiating a contraction. Shocking on a T wave is like trying to breathe out when you’ve already emptied your lungs. You can’t breathe out anymore because you have to breathe in first. The shock prevented the ions from coming back into the cells. They must repolarize so that they can depolarize.
When is Synchronized Cardioversion Used?
Use this method when your patient has a rapid heartbeat that is somewhat organized. Organized arrhythmias include:
- Atrial fibrillation (AFib)
- Atrial flutter
- Ventricular tachycardia (VTach)
- Supraventricular Tachycardia (SVT)
This technique is also part of the protocols you’ll learn in ACLS (Advanced Cardiac Life Support) and PALS (Pediatric Advanced Life Support) courses. This 100% online training from Advanced Medical Certification teaches you the precise moments when synchronized cardioversion is the best treatment. Whether you’re managing an emergency in the ER or treating a patient in an ambulance, knowing when to act—and how—can make all the difference.
Let’s take a closer look at these indications for synchronized cardioversion. Here are the core rhythms treated with this procedure.
Atrial Fibrillation (AFib)
AFib is one of the most common arrhythmias treated with synchronized cardioversion. In AFib, the upper chambers of the heart (the atria) beat irregularly and rapidly, causing poor blood flow. The left atrium doesn’t fill completely before sending blood to the left ventricle on its way to the lungs. At the same time, the oxygenated blood returning to the heart doesn’t fill the right atrium before being sent to the right ventricle. The heart is working harder than it should have, and as it tries to keep up with the demand, heartbeats become irregular.
If your patient has AFib and medications aren’t working, synchronized cardioversion can help restore a regular heart rhythm. This is crucial to prevent complications like stroke or heart failure.
Ventricular Tachycardia (VTach)
VTach is another arrhythmia that requires urgent treatment. VTach occurs when the lower chambers of the heart (the ventricles) beat too quickly, leading to inefficient pumping of blood to the lungs and then out to the body. Most often, VTach calls for a timed shock. However, I’ll share an exception in the next section, so read on!
These exceptions are why it’s essential to study life-saving algorithms. They guide you through critical decision-making so you can feel confident in making a split-second judgment on what to do next.
Atrial Flutter
Similar to AFib, atrial flutter is a rapid, organized arrhythmia that affects the atria. The heart may beat fast but in a regular pattern. If your patient is symptomatic or unstable, synchronized cardioversion can correct the rhythm and prevent further complications.
Supraventricular Tachycardia (SVT)
This refers to rapid heartbeats originating above the ventricles, often in the atria. SVT can cause symptoms like palpitations, dizziness, or chest pain. If medications don’t work, synchronized cardioversion can restore a normal heart rhythm.
Synchronized cardioversion is used when the patient is stable but showing symptoms. Your quick action is vital to prevent VTach from progressing to ventricular fibrillation.
In ventriclar fibrillation (VFib) the ventricles become so uncoordinated that very little blood makes it out to the body. This is a life-threatening emergency. VFib is one of the most common causes of sudden cardiac death.
To apply this information effectively, you must know how to identify rhythms. You’ll find this free ACLS training helpful if you need a refresher.
Synchronized Cardioversion vs Defibrillation
Both procedures deliver shock to the heart. However, they serve different purposes.
You’ll use synchronized cardioversion to treat organized arrhythmias (outlined above) with a timed shock. Deliver the shock at the safest moment, which is the R Wave (depolarization phase) on the ECG, to avoid triggering a dangerous arrhythmia like VFib.
On the other hand, you’ll use what I’ll call regular defibrillation when the heartbeat is already disorganized or your patient has pulseless VTach, that exception I mentioned earlier. To give this patient the best chance of survival, you are prioritizing delivering shock immediately over trying to time it because the brain isn’t getting any oxygen.
In defibrillation, the only timing decision involved is determining if your patient has a shockable rhythm, pulseless ventricular tachycardia (pVT) and ventricular fibrillation (VF)
Synchronized Cardioversion vs. Unsynchronized Cardioversion
Unsynchronized cardioversion is simply another name for defibrillation without precise timing. When you take an ACLS course, these terms may be used interchangeably in the study materials or the test.
Synchronized Cardioversion Joules in ACLS (for Adults)
In ACLS protocols for adult tachycardia, the recommended energy levels for synchronized cardioversion vary based on the arrhythmia. You’ll typically begin with the lowest indicated joules before increasing for subsequent shocks.
Here’s a quick guide for patients with tachycardia and a rhythm that calls for this procedure.
Narrow Regular: 50 to 100J
A narrow QRS complex describes electrical activity that is primarily occurring in the atria or above the ventricles while the heartbeat is fairly predictable.
This might be the case with Supraventricular Tachycardia (SVT).
Narrow Irregular: Biphasic 120J to 200J / Monophasic 200 J
This also describes electrical activity in the atria or above but with an irregular rhythm.
Wide Regular: 100J
A Wide QRS complex indicates electrical activity coming from the ventricles, and the rhythm is fairly regular.
Wide irregular: Defibrillation Dose (NOT Synchronized)
Wide QRS complex again refers to ventricular-origin electrical activity, but the beats are erratic to the point of unpredictability. Synchronized is not called for here.
Examples might include Ventricular Fibrillation (VFib) or pulseless VTach.
Synchronized Cardioversion Joules in PALS (for Children)
When administering a shock to a child, it’s important to follow your PALS training. If you have the potential to work with children in an emergency setting, you should definitely get PALS certified. You can do it 100% online in a convenient self-paced course and earn continuing medical education credits to put toward your license renewal.
For children, you need to know (or make an educated guess) about the child’s weight. Administer .5 -1 joules per kg. If it fails to correct the heart rhythm, increase to 2 joules per kg. For those who don’t think in metrics, 1kg is 2.2lb.
So, a 60lb child (perhaps an 8-10 year old) weighs 27kg (rounded). 27kg x .5J to 1J = 13.5J – 27J
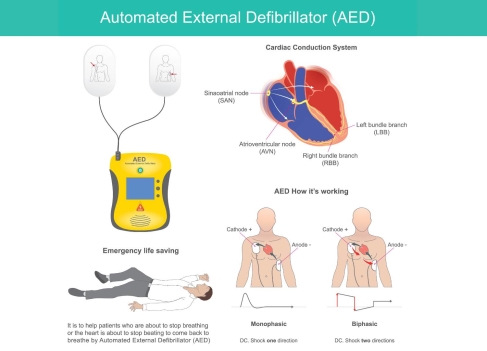
How Do I Use AED for Synchronized Cardioversion
Some advanced AEDs (automated external defibrillators) have a synchronized cardioversion mode. If you’re in an out-of-hospital setting where an AED is available, you’ll need to confirm that the device has this feature. Follow the prompts from the AED, and ensure it’s set to “sync” mode before delivering the shock.
Your ACLS certification will increase your confidence in manual defibrillators and AEDs, ensuring you’re ready to act in any situation with any tool you might have.
Step-by-Step Cardioversion Procedure
1. Monitor and Assess
Connect your patient to the cardiac monitor to observe their ECG and identify the type of arrythmia. Determine if your patient’s rhythm is suitable for this procedure.
2. Prepare the Defibrillator
Set up your defibrillator (which could be an AED) to synchronized mode. Then, select the appropriate energy level.
At this time, consider vagal maneuvers before proceeding. In patients with Supraventricular tachycardia (SVT), these non-invasive techniques activate the parasympathetic nervous system, telling the heart to slow down. This is safer and can slow the heart down, allowing it to re-establish a normal rhythm on its own. (NIH.gov)
3. Consider Sedation for Synchronized Cardioversion
This is a painful and potentially anxiety-inducing procedure, and the patient is probably awake and aware if they have an appropriate rhythm. Use a drug like midazolam (a sedative) or propofol (an anesthetic) to quickly sedate them or dull the pain. (NIH.gov). The drugs used vary by country, clinic, and situation, so you should review your facilities’ guidance here.
4. Position the Pads
Place the pads on the patient’s chest according to the manufacturer’s instructions ((anterior-posterior or anterior-lateral positions).
5. Charge the Defibrillator
Charge the defibrillator to the selected energy level based on the type of arrhythmia. Again, review ACLS algorithms for more details.
6. Clear the Area
Ensure no one is touching the patient or the bed. Loudly announce “Clear” before delivering the shock to your patient in the next step.
7. Shock
Press the “shock” button, and the defibrillator will synchronize with the R wave and deliver the shock to your patient at the safest moment.
8. Monitor and Reassess
Immediately check your patient’s rhythm to determine if you need to shock again. If the arrhythmia persists, increase the energy level and repeat the procedure. If the rhythm normalizes, monitor the patient.
Post-sedation care is critical here. The patient must be closely monitored until they are fully awake and stable.
Risks and Side Effects of Synchronized Cardioversion
Knowing the risks can help you anticipate how your patient may react to the procedure. This allows you to prepare for several potential outcomes.
- Skin Burns: The electrical shock may burn your patient’s skin. Proper placement of pads and gel can reduce this risk. However, you should evaluate the patient’s skin to treat burns after, as necessary.
- Worsening Arrhythmias: In some cases, your patient’s arrhythmia may worsen into ventricular fibrillation (VF). Shocking on the T wave should prevent this, but it can happen.
- Stroke Risk: If your patient has Afib, they may experience a blood clot, which could lead to a stroke. When time allows, your Afib patient should receive anticoagulants for several weeks before the procedure to prevent this.
- Hypotension (Low Blood Pressure): Your patient’s blood pressure could drop into bradycardia after the procedure, making post-intervention monitoring critical.
- Cardiac Arrest: This one is rare because of the precise timing of the shock. However, the heart could stop. If it does, you’ll need to follow what you learned in ACLS training or PALS if your patient is a child.
If the patient is/was sedated, they may also experience confusion, nausea, and trouble waking up.
Be Ready for Demanding Medical Situations with Advanced Training
Advanced medical training from Advanced Medical Certification prepares you for emergency situations like these. Algorithms that follow ILCOR’s evidence-based protocols guide you through the decision-making process while reminding you of the proper steps, considerations, and doses. Online PALS and ACLS Megacodes help you apply what you learned before facing a real-life emergency.
To earn continuing medical education credits and update your skills with the latest evidence-based procedures, get the PALS/ACLS bundle to save money while you save lives.