2020 ILCOR Guidelines: What Has Changed?
2020 ILCOR Guidelines: What Has Changed?

by Greta Kviklyte
Life Saver, AMC
Co-authored by Kim Murray, RN, M.S.
posted on Mar 8, 2021, at 7:04 am
Whether you are providing first aid, basic life support or another resuscitative service, following the appropriate algorithm or protocol is essential. These guidelines were established based on the results of research, as well as a body of knowledge developed through decades of practice. Learning all of these guidelines and being able to recall them during emergency situations is key to providing effective care and potentially life-saving treatment. However, it is also important to note that these guidelines are subject to change. As the medical community gains more knowledge, new discoveries are made, and these guidelines may be altered in hopes of improving outcomes.
We offer Online CPR and BLS Certification
In 2020, the International Liaison Committee on Resuscitation published new guidelines containing several notable changes to systems of care, including altered life support and first aid algorithms. Changes were most notable for first aid, infant/child CPR, adult basic life support, advanced life support. Read the blog and watch the video below to learn more.
Updates to Pediatric Basic Life Support
When providing CPR to infants or small children, it is now recommended to perform 15 chest compressions, followed by 2 breaths. This is considered one “cycle” and should be continued until more sophisticated life-saving measures are available. Prior to these changes, recommendations were to give 30 compressions and two gentle breaths per cycle.
The 2020 update also alters the recommendations for providing life support to infants and children who have a pulse but have absent or inadequate breathing. The ILCOR recommends giving one breath every two to three seconds, which translates to 20 to 30 breaths per minute. In the past, the recommendation was to administer rescue breaths at a rate of one breath every three to five seconds, which would have translated to only 12 to 20 breaths per minute.
Full Updated Pediatric Basic Life Support Algorithm
The complete 2020 updated Pediatric Basic Life Support algorithm is as follows:
- Verify that the patient is unresponsive with abnormal or absent respiration.
- Call 911/EMS; Locate an AED or defibrillator if possible.
Assess the patient’s pulse. - If the patient has a weak pulse, administer one breath every three seconds. Add chest compressions if the pulse remains below 60 beats per minute. Assess the patient’s pulse every 2 minutes.
- If the patient has no pulse, begin CPR cycles of 15 compressions and 2 rescue breaths.Once an AED becomes available, assess the patient for a shockable rhythm.
- If the rhythm is shockable, administer one shock and resume CPR for 2 minutes before re-assessing rhythm.
- If the rhythm is not shockable, resume CPR and reassess rhythm every 2 minutes.
- Steps should be continued until more advanced life-saving measures are available or the patient shows evidence of a return to normal circulation.
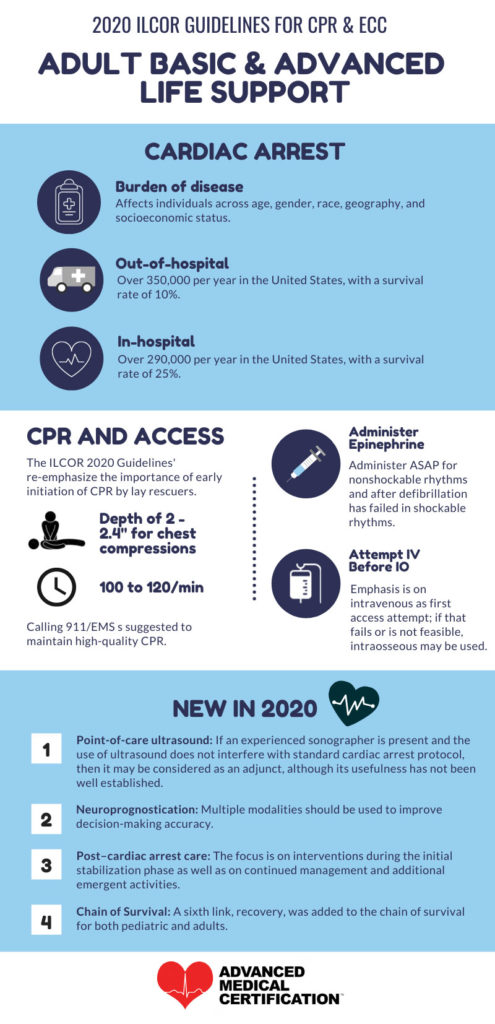
Changes to Adult Basic and Advanced Life Support Algorithms
The ILCOR 2020 guidelines for Adult Basic and Advanced Life Support have also undergone some changes. The ILCOR re-emphasized the importance of initiating CPR quickly in cases where someone experiences cardiac arrest outside the hospital. The most recent studies show that, while in-hospital cardiac arrests have a survival rate of 25 percent, out-of-hospital cardiac arrests have a survival rate of only 10 percent. The ILCOR also emphasized the importance of performing chest compressions to a depth of 2 to 2.4 inches. Compressions should be performed at a rate of 100 to 120 per minute. In addition, the ILCOR 2020 guidelines emphasize the importance of administering epinephrine for non-shockable rhythms, as well as after defibrillation has failed in a shockable rhythm.
New to the ILCOR 2020 guidelines for Adult Basic and Advanced Life Support Algorithms were the following:
- Point-of-care ultrasound changes: If an experienced sonographer is available, and if performing an ultrasound will not interfere with other life-saving measures, ultrasound can be used to provide additional information about the function of the heart and the cause of cardiac arrest during life support. However, research has not yet established the usefulness or effectiveness of this strategy.
- Changes to the chain of survival: A sixth link has been added to the chain of survival. This link is “recovery”, and it includes observation, rehabilitation, psychological support and any other services the patient may need. This change applies to both adult and pediatric life support.
- Post-cardiac arrest care: The focus of post-cardiac arrest care is on interventions during the initial stabilization phase. Continued management is also emphasized.
- Neuroprognostication: When predicting neurological recovery and planning patient care, the ILCOR recommends using multiple modalities to improve the accuracy of decisions.
Full Updated Adult Basic Life Support Algorithm
The complete 2020 updated Adult Basic Life Support algorithm is as follows:
- Verify that the patient is unresponsive and has abnormal respiration.
- Call 911/EMS; Locate an AED if possible.
- Assess the patient’s pulse.
- If the patient has a pulse but respirations are absent or abnormal, administer one rescue breath every five to six seconds. Reassess pulse every two minutes.
- If the patient has no pulse and respirations are absent or abnormal, start cycles of 30 chest compressions and two rescue breaths.
After a defibrillator/AED becomes available, assess the patient for a shockable rhythm. - If the rhythm is shockable, administer one shock and resume CPR for two minutes and reassess rhythm.
- If the rhythm is not shockable, resume CPR for two minutes and reassess rhythm.
- Steps should continue until more advanced life-saving measures are available or the patient shows evidence of a return to normal circulation.
It is important to begin chest compressions within ten seconds whenever possible. Chest compressions should be hard and fast, while allowing for a complete recoil of the chest between compressions. Rescue breaths should cause the chest to rise.
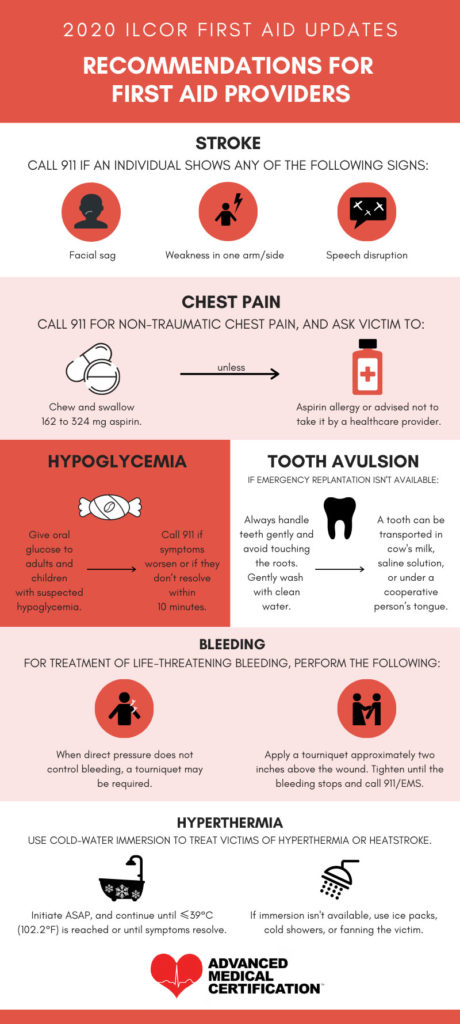
Changes to First Aid Recommendations
Several changes were made to ILCOR first aid recommendations. The changes, updates, and emphases are as follows:
- Strokes – Stroke should be suspected in cases where a patient shows evidence of one-sided facial weakness, one-sided arm weakness and/or speech disruption. When these signs occur, call 911 immediately.
- Chest Pain – When a patient is experiencing chest pain unrelated to trauma, call 911. Next, ask the patient to chew and swallow 162 mg to 324 mg aspirin. If the patient has an allergy to aspirin or has been advised not to take this medication, do not administer aspirin. Instead, simply wait for help to arrive.
- Hypoglycemia – Patients with suspected hypoglycemia should be given glucose orally. If symptoms worsen or do not resolve within 10 minutes, call 911. Symptoms of hypoglycemia may include elevated heart rate, hunger, sweating, dizziness, and confusion.
- Tooth Avulsion – If emergency replantation is not a possibility, collect the tooth gently and avoid touching the root. Wash the tooth carefully with water. For safe transport, place the tooth in a saline solution, in cow’s milk, or under the patient’s tongue, as long as the patient is a cooperative adult. Pediatric patients should not be asked to hold a tooth under the tongue, as this may put them at risk of airway obstruction.
- Bleeding – If a patient is experiencing life-threatening bleeding, try to control bleeding with direct pressure. If direct pressure does not control the bleeding, apply a tourniquet. The tourniquet should be placed approximately two inches above the wound. Tighten the tourniquet until the bleeding has stopped and call 911 for assistance.
- Hyperthermia – Hyperthermia occurs when someone’s temperature rises above safe levels, leading to rapid heart rate, nausea, vomiting, dizziness, confusion, and other symptoms. When someone is suspected to be a victim of hyperthermia or heatstroke, immerse the victim in cold water immediately. Keep the victim immersed in cold water until their temperature is no higher than 102.2 degrees Fahrenheit or until the victim’s symptoms have resolved. If immersion in cold water is not possible, use fanning, cold showers and/or ice packs to lower the victim’s temperature.
Other Changes and Updates
- Double sequential defibrillation is no longer recommended based on the most recently available data.
- ILCOR guidelines state that continuously measuring the patient’s arterial blood pressure and ETCO2 during ACLS resuscitation could improve CPR outcomes.
- During ACLS resuscitation, the preferred route of administering medication is intravenous access. If IV access is not a possibility, intraosseous access is acceptable.
- Following resuscitations, ILCOR guidelines recommend a debriefing for those involved in the event for the purpose of supporting their well-being and mental health.
- When providing life support services to pregnant women, the primary focus is on resuscitating the mother. Preparations for perimortem cesarean delivery should also be made if it would be necessary to improve the chances of resuscitating the mother and/or to save the infant.
- Recovery from an incident of cardiac arrest is a lengthy process, continuing long after the patient’s initial hospitalization. ILCOR guidelines recommend providing patients with a formal assessment, as well as support for their cognitive, physical, and psychosocial needs.
- When providing care to patients after the return of normal circulation, ILCOR guidelines recommend paying close attention to blood pressure, oxygenation, and body temperature. Patients should also be evaluated for percutaneous coronary intervention.
The ILCOR guidelines also introduced a new Cardiac Arrest in Pregnancy Algorithm, as well as two new Opioid-Associated Emergency Algorithms to help with these specific, unique cases.
The Importance of Up-to-Date Information
Any changes to the ILCOR guidelines are made based on new knowledge gained, either through experience or through research. In many cases, data analysis is the primary driving factor behind these changes. The goal of these changes is always to improve the quality of life support, which in turn improves survival rates and patient outcomes. When laypeople or healthcare providers who may need to administer life support are aware of these changes, they can provide the best possible services to individuals who experience cardiac arrest or other types of medical incidents.
Because these guidelines change on a regular basis, it is important for anyone who hopes to provide life support in the future, as well as those who must be trained to provide life support services as a part of their employment, to keep up with any changes that are made. This is one of the reasons most healthcare employers require their employees to recertify their life support credentials at regular intervals.
The easiest way to make sure that you are always using the recommended algorithms and protocols when providing life support or first aid is to update your credentials as required by your employer. If you are not subject to these requirements, simply update your credentials before their expiration date to keep your skills honed. You should also take a course and update your life support credentials whenever you learn that the guidelines have changed substantially.
How To Update Your Life Support Credentials
Whether you want to recertify your life support credentials as a requirement for continued employment or for your own peace of mind, you can complete this task easily by taking a life support course. Both in-person and online options are available. However, because of the many benefits, many people are now choosing to take their life support courses online. Taking the course online allows you to progress through the materials at your own pace and in the comfort of your own home. You won’t have to follow anyone else’s schedule, and you won’t have to worry about traveling to a physical class or interacting with teachers and students in person. This option is ideal for people who have busy or unpredictable work schedules, as well as those who simply don’t want the hassle of an in-person course.
Advanced Medical Certification offers a range of life support courses, including First Aid, CPR, BBP, BLS, PALS and ACLS. All of our courses are conducted 100 percent online, and you will never be asked to come to a classroom. In addition, your credentials will be available immediately after you have passed the course. If you don’t pass the exam on the first try, you can take it as many times as necessary until you are able to get a passing score. Our credentials are accepted by the majority of employers, allowing you to satisfy your requirements easily. We also offer 3 course and 2 course bundles to make our courses more affordable. Contact us today to learn more.




thank you for the 2020 bls update
You are welcome, Fatima 🙂