Essential Insights: Normal Respiratory Rates for Kids & Adults
Essential Insights: Normal Respiratory Rates for Kids & Adults

by Greta Kviklyte
Life Saver, AMC
Co-authored by Kim Murray, RN, M.S.
posted on Dec 29, 2021, at 5:52 am
In emergency situations, being able to recognize quickly whether a person is suffering from respiratory distress is critical to ensure that life-saving measures are implemented as soon as possible.
Children and adults suffering from respiratory distress will typically present with similar signs and symptoms, but there are significant differences between normal respiration in a child vs an adult. Understanding these differences will assist the professional rescuer (or bystander) in providing effective emergency care.
This article discusses important things to know about the normal respiratory rate in children, the common causes, signs, and symptoms of pediatric respiratory distress, complications associated with respiratory distress, and how to manage or treat breathing problems in a child.
We offer Online PALS Certification and Renewal
But first, a review of important definitions, as well as a very brief summary of the respiratory system itself, should add some helpful context to this discussion.
Helpful Definitions
- Respiratory failure: a condition in which blood does not have enough oxygen and/or too much carbon dioxide; can be chronic or acute
- Respiratory distress: an emergency medical condition in which a person is struggling to breathe
- Ventilation: the mechanical act of breathing in which air flows into the lungs (inhalation) and out of the lungs (exhalation)
- Respiration: the physiological effect of breathing in which gas (e.g., oxygen and carbon dioxide) is exchanged between the environment and cells in the body
- Hypoxemia: not enough oxygen in the blood
- Hypercapnia: too much carbon dioxide in the blood
The Respiratory System 101: Parts and Process
 The main goals of the respiratory system are to bring oxygen into the body and expel carbon dioxide out of the body. Some of the main structures involved in the respiratory system include, but are not limited to, the following:
The main goals of the respiratory system are to bring oxygen into the body and expel carbon dioxide out of the body. Some of the main structures involved in the respiratory system include, but are not limited to, the following:
- Mouth and nose
- Sinuses: hollow spaces between bones in the head that help regulate humidity and temperature of inhaled air
- Pharynx (throat): the tube-like passageway through which air travels from the mouth and nose to the trachea
- Trachea (windpipe): the tube-like passageway that connects the throat and lungs
- Bronchial tubes: major tube-like passageways that are found at the bottom of the trachea and connect to each lung
- Lungs: the two organs, divided into lobes or sections (three lobes on the right lung and two lobes on the second lung), that fill with air and allow gases to exchange between air and blood
- Alveoli: tiny air sacs in the lungs
- Bronchioles: smaller tubes through which air flows from the bronchial tubes to the alveoli
- Diaphragm: a tent-like muscle beneath the lungs that helps airflow in and out of the lungs
What Happens When You Breathe?
The following is the basic process of what happens during inhalation and exhalation:
- As a person breathes in, the diaphragm moves down and the ribs move up and out. This helps the chest area become bigger, so the lungs have room to expand. This also decreases the pressure inside the alveoli so that air flows into the lungs (air, like other gases, moves from areas of higher pressure to lower pressure).
- Oxygen in the air moves from the alveoli into the blood flowing inside tiny blood vessels called capillaries, which are located inside the alveolar walls.
- Once inside the blood, oxygen attaches to proteins on red blood cells called hemoglobin. The heart pumps this oxygen-rich blood around the body in blood vessels called arteries.
- As cells and tissues in the body receive and use oxygen from the blood, they send off carbon dioxide into the blood.
- This carbon dioxide-rich blood flows back to the heart in blood vessels called veins, and then the heart pumps this carbon dioxide-rich blood back to the lungs.
- Carbon dioxide moves from the capillaries back into the alveoli. As a person breaths out, the diaphragm moves up and the ribs move down. This helps the chest area become smaller and increases the pressure inside the lungs, allowing air to get pushed out.
What Is a Normal Respiratory Rate for Adults?
The normal respiratory rate for adults is between 12 and 18 breaths per minute at rest. If respiration rates are under 12 breaths per minute, a person may not get enough oxygen to meet their body’s needs. Respiratory rates over 25 can indicate an underlying health condition or trouble breathing.
What is a Normal Respiratory Rate for a Newborn?
Newborns have a much faster normal respiratory rate than adults. Typically, babies will breathe at a rate of 40 to 60 times per minute at a normal breathing rate. As the baby falls asleep, their breathing rate may fall to between 30 and 40 times per minute. Breathing faster than adults is not a sign of a health complication for newborns unless it is beyond 60 times per minute. Children who are born early or with other health complications may have a breathing rate that is much outside of this range, and that could indicate underdeveloped lungs.
The Normal Respiratory Rate in Children
 he respiratory rate refers to the number of times a person breathes in one minute while at rest (i.e., not performing exercise or physical activity). The normal respiratory rate in a child tends to be quicker than an adult’s.
he respiratory rate refers to the number of times a person breathes in one minute while at rest (i.e., not performing exercise or physical activity). The normal respiratory rate in a child tends to be quicker than an adult’s.
Understanding the normal breathing rate for children can help a professional or bystander rescuer more quickly recognize whether a child is suffering from breathing difficulties.
Typical respiratory rates for children, based on age range, are as follows:
- Infant (0-12 months old): 30 to 60 breaths per minute
- Toddler (1-3 years old): 24-40 breaths per minute
- Preschooler (4-5 years old): 22-34 breaths per minute
- School-aged child (6-12 years old): 18-30 breaths per minute
By the time a child reaches adolescence (13 to 18 years old), their normal respiratory rate will be the same as an adult’s—about 12 to 16 breaths per minute.
Interestingly, infants and young children also tend to have faster heart rates (pulses) than adults on average. The normal resting heart rate of a newborn (0 to 3 months old) ranges from 80 to 205 beats per minute, and a child aged 4 months to 2 years has a normal resting heart rate of 75 to 190 beats per minute. Between ages 2 and 10, a child’s heart rate will slow to about 70 to 140 beats per minute.
By the time she is 10 years old, a child’s resting heart rate will be similar to an adult’s (60 to 100 beats per minute).
Why Do Children Breathe Faster Than Adults?
Generally speaking, children tend to breathe faster than adults do because they have smaller lungs (lower lung volume) than adults, and therefore have less physical space to exchange gases.
Younger children also tend to have a much faster metabolism than adults, meaning they break down nutrients at a faster rate. As a result, children typically require more oxygen (and faster disposal of carbon dioxide) while at rest compared to adults, even after adjusting for body mass and unit of time.
What Is a Low Respiratory Rate?
A low respiratory rate is typically under 12 breaths per minute for adults or under 20 breaths per minute for children. Newborns should not be below this figure, though some slightly older children may be.
A low breathing rate indicates that the body may not be getting enough oxygen to meet its needs. Too low a respiratory rate is called bradypnea, and it requires immediate medical attention.
What Is a High Respiratory Rate?
A high respiratory rate occurs when a person breathes very quickly, often not getting deep breaths. This condition, called tachypnea, can mean not enough air is getting into the lungs to meet the body’s needs. In adults, breathing rates of over 25 breaths per minute can be problematic, and in children, breathing rates over 40 breaths per minute in most children or 60 breaths per minute in newborns can indicate complications.
What Should Your Respiratory Rate Be While Sleeping?
While a person sleeps, the rate of breathing slows because the need for a higher amount of oxygen is less. However, the normal respiratory rate during sleep periods should not drop below the lowest levels listed above based on the individual’s age.
How to Measure Respiratory Rate
To measure respiratory rate or breathing rate, follow these steps:
- Monitor the person for a few seconds to better understand how they are breathing. The patient should sit or lie but remain still during this period.
- Count the movements of the chest as it rises or falls. Every time it rises, it indicates one breath.
- Monitor this rate over 1 minute while watching a clock or a watch.
This indicates the number of breaths per minute.
What Conditions Affect Your Respiratory Rate?
A range of conditions exist that could influence the rate at which you are breathing. Some of the most common include:
- Chronic obstructive pulmonary disorder (COPD)
- Anxiety
- Heart failure
- Pneumonia
- Carbon monoxide poisoning
- Asthma
- Medications taken
- Fever or infection
- Pulmonary embolism
- Respiratory conditions such as the common cold or flue
- Dehydration
- Chronic smoking
- Pain
- Anemia
Causes of Abnormal Respiratory Rates in a Child
Common causes of abnormal breathing or respiratory distress in children include the following:
- Bacterial or viral infections, including croup or pneumonia
- Allergies
- Asthma
- Exposure to cigarette smoke or other harmful gases, including pollution and carbon monoxide
- A blocked airway (choking)
- Trauma or damage to any part of the respiratory system
- Complications from medications (e.g., accidental overdose)
- Certain genetic conditions, including cystic fibrosis
Signs and Symptoms of Pediatric Respiratory Distress
As a general rule, a child who is consistently taking fewer than 10 breaths per minute or greater than 60 breaths per minute is likely suffering from some sort of respiratory distress and requires immediate attention.
Beyond assessing a child’s respiratory rate, you can also look for other key signs and symptoms of pediatric breathing problems. These signs and symptoms include:
-
- Changes in skin quality: a child’s skin (especially around the lips, hands, and feet, including the nail beds) might become pale, purplish, grayish, or bluish in color, and could start to feel cold and clammy
- Nasal flaring: the nostrils open wide when breathing in
- Chest retraction: with each breath, the chest appears to sink in just below the neck or beneath the breastbone
- Noisy breathing: a child might begin to make unusual sounds while breathing, including
- Wheezing (a high-pitched, whistling, musical-like sound that usually only happens on exhalation and usually suggests a narrowing in the lower airway)
- Stridor (a special kind of high-pitched wheezing noise that can occur during exhalation or inhalation and usually suggests an obstruction or narrowing in the upper airway)
- Stertor (a snoring-like sound that often develops when a child has congestion in the mouth or nose)
- Grunting (“ugh” sound)
- Changes in mood or level of alertness: the child might become drowsy, anxious, restless, difficult to arouse, or simply not like themselves
- Changes in body position: a child may spontaneously lean forward or tilt their head up or backwards in an attempt to make breathing easier (if a child is choking, he or she may also exhibit the universal sign of choking by placing their hands at their throat)
Untreated, respiratory distress can be fatal or lead to life-threatening or life-altering complications including organ damage, shock, anoxic brain injury, and nervous system depression due to increased carbon dioxide levels in the blood.
Importance of Respiratory Rate in Health
Maintaining the normal respiratory rate for adults and children is critical to health and well-being. Any range outside of the normal respiratory rate indicates that a person’s lungs are not getting enough oxygen to meet the body’s needs. Low respiratory rates often mean the lungs are not breathing in enough air, while a high breathing rate indicates shallow breaths that may not provide enough oxygen. Maintaining normal respiratory rates can greatly enhance the overall function of the brain and other organs.
How to Monitor Your Respiratory Rate
 The only way to monitor your breathing rate manually is to count the number of breaths you have while at rest. Once you learn how to measure your respiratory rate (as noted above), you can track your breathing rate over time to notice differences.
The only way to monitor your breathing rate manually is to count the number of breaths you have while at rest. Once you learn how to measure your respiratory rate (as noted above), you can track your breathing rate over time to notice differences.
Monitor Respiratory Rates for Children
If you are unsure if your child is getting the normal respiratory rates they need, monitor them to notice changes in breathing rate and function. For example, if your child seems to be breathing heavily or wheezing, that could indicate a lung concern. If you see any of the above-mentioned symptoms, have the child sit down and count their breaths. You can also monitor their respiratory rate during sleep to ensure they are safe. If you do not see normal respiratory rates, consider further investigation to determine if the child is experiencing a health concern.
How to Improve Your Respiratory Rate
If your normal respiratory rates are higher than normal, you can work to improve these rates. To do so, you’ll need to improve overall fitness levels and learn to breathe deeper. In terms of breathing rates, practice makes improvement possible – deep breathing, counting your breaths, and watching your posture can also help.
What Is the Correct Ventilation Rate for a Pediatric Patient in a Respiratory Arrest?
The correct ventilation rate for a pediatric patient is 1 ventilation for every 2 to 3 seconds.
When to Seek Medical Help
When the normal respiratory rates are not met, as noted above by age, it is important to seek medical care. This is especially important when it occurs for more than a few minutes. There is often the need to take corrective action to supply more oxygen to the brain in these situations. A breathing rate while sleeping below the standard levels listed above is indicative of the need for oxygen.
Pediatric vs. Adult Respiratory Rates
The following chart shows normal respiratory rates for children and adults, as well as for newborns, toddlers, and older children.
Respiratory Rates for Children |
|
| Age Range | Breaths per Minute |
| Infant (0-12 months) | 30-60 breaths per minute |
| Toddler (1-3 years old) | 24-40 breaths per minute |
| Preschooler (4-5 years) | 22-34 breaths per minute |
| School-aged child (6-12 years old) | 18-30 breaths per minute |
| Adolescence (13-18 years old) | 12-16 breaths per minute |
| Adult | 12-18 breaths per minute |
What To Do If a Child is In Respiratory Distress (Child vs Infant)
 If there is any concern that a child is suffering from respiratory distress, call 911. If a child passes out, begin cardiopulmonary resuscitation (CPR). Importantly, rescuers who are alone should perform CPR on a child for at least 2 minutes before stopping to call 911.
If there is any concern that a child is suffering from respiratory distress, call 911. If a child passes out, begin cardiopulmonary resuscitation (CPR). Importantly, rescuers who are alone should perform CPR on a child for at least 2 minutes before stopping to call 911.
Recall that the CPR techniques used on a baby or prepubescent child (aged 1 to 12 years) have some differences compared to the CPR technique used on an adult. Some of the main differences include the following:
- For infants, the depth of chest compressions – which can be done with two fingers at the center of the baby’s chest as a single rescuer – should be about one and a half inches (vs two inches for children and adults)
- Care should be taken not to tip the infant’s or child’s head back too far nor provide rescue breaths that are too forceful
- Checking a child’s pulse should be performed at the carotid artery (side of the neck), as it is for adults; in infants, the pulse should be checked at the brachial artery (inside of the bicep)
In the case of known or suspected airway obstruction (choking), back blows and/or the abdominal thrust maneuver may be indicated to help the child clear the foreign object.
If a child older than 1 year old is choking, you can provide the same type of abdominal thrust maneuver that would be performed on an adult.
- First ensure the child is actually choking – look for choking signs and symptoms and ask them, “Are you choking? Can you talk?” If the child is able to speak and cough forcefully, do not begin first aid, as the child may still be able to dislodge the obstruction on their own. If the child is unable to talk or not able to produce a strong and effective cough, proceed with the rescue maneuver.
- If the child is much shorter, the rescuer should kneel, not stand, behind the choking victim.
- Wrap your arms around the child’s waist.
- Place one fist, thumb side in, just above the child’s belly button.
- Grab your fist with your other hand.
- Make quick upward and inward movements with your hands, as if you were trying to lift the child up.
For choking children and adults, the American Red Cross recommends using the “five-and-five” approach, in which the rescuer alternates between five black blows and five abdominal thrusts. The rescuer should continue this approach until the object is dislodged, the child begins coughing forcefully again, or the child passes out.
If an infant younger than 1-year-old is choking, a different technique is required (all of these techniques are discussed in detail in BLS training courses and related certifications). To do:
- Hold the infant face down against your forearm and support the infant’s head and neck securely using your hand. Be sure to keep the infant’s head lower than the chest. If able, support your arm by resting it against your thigh.
- Use the heel of your other hand to give the child five quick forceful blows between the shoulder blades.
- Carefully flip the infant over so that she is resting on her back.
With your other hand, place two fingers on the center of the infant’s chest, just below the nipples. Press your fingers inward quickly five times.
Share your experience of assisting someone in respiratory distress.
Normal Respiratory Rates Are Critical to Know
- The normal respiratory rate for adults is 12 to 20 per minute and differs for children based on age.
- A low respiratory rate could mean that a person is not getting the oxygen they need.
- Knowing the difference in normal respiratory rates for adults and children allows you to know when to take action.
Are You Prepared To Care for a Child in Respiratory Distress?
If you’re a healthcare provider or an employer, contact Advanced Medical Certification today to learn about our online certification and recertification courses in Pediatric Advanced Life Support (PALS) and other courses.




 For non-medical professionals and laypeople, BLS and other advanced lifesaving certifications aren’t necessary. However, CPR and basic first aid are extremely valuable skills for anyone to know. Individuals who choose to learn CPR and basic first aid could end up saving a life someday—including the life of someone they love or work with.
For non-medical professionals and laypeople, BLS and other advanced lifesaving certifications aren’t necessary. However, CPR and basic first aid are extremely valuable skills for anyone to know. Individuals who choose to learn CPR and basic first aid could end up saving a life someday—including the life of someone they love or work with. BLS certifications must be renewed every two years. This is to ensure essential lifesaving skills and knowledge are retained, which can help improve outcomes for people suffering from life-threatening emergencies.
BLS certifications must be renewed every two years. This is to ensure essential lifesaving skills and knowledge are retained, which can help improve outcomes for people suffering from life-threatening emergencies. The normal resting heartbeat of an adult is between 60 and 100 beats per minute. The normal resting heart rate of an infant (birth to about 3 months of age) ranges from
The normal resting heartbeat of an adult is between 60 and 100 beats per minute. The normal resting heart rate of an infant (birth to about 3 months of age) ranges from 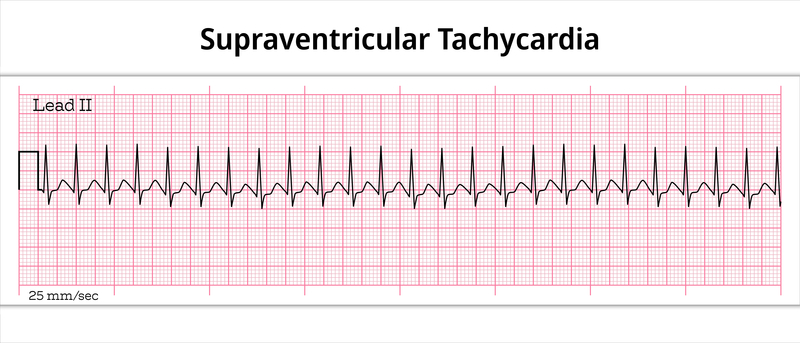 In a
In a  While you may wish to learn how to lower your heart rate using a supraventricular tachycardia vagal maneuver, some risks go along with it.
While you may wish to learn how to lower your heart rate using a supraventricular tachycardia vagal maneuver, some risks go along with it. While they are simple, non-invasive, and generally effective, vagal maneuvers are not without risk. Patients should never attempt vagal maneuvers without the supervision of a medical provider.
While they are simple, non-invasive, and generally effective, vagal maneuvers are not without risk. Patients should never attempt vagal maneuvers without the supervision of a medical provider. Medical assistants usually take medical histories and vitals from patients. They may assist in more advanced ways like drawing blood and providing first aid as their skills advance. You may also handle important administrative, clerical and clinical tasks as you learn more on the job. You might work in a doctor’s office, community clinic, hospital, or another clinical setting.
Medical assistants usually take medical histories and vitals from patients. They may assist in more advanced ways like drawing blood and providing first aid as their skills advance. You may also handle important administrative, clerical and clinical tasks as you learn more on the job. You might work in a doctor’s office, community clinic, hospital, or another clinical setting. While there are no certifications required to become a medical assistant, the material you learn in programs will be extremely beneficial to you and your potential employers. Certification helps you practice to the highest degree, whether you are training to become a medical assistant or a surgeon!
While there are no certifications required to become a medical assistant, the material you learn in programs will be extremely beneficial to you and your potential employers. Certification helps you practice to the highest degree, whether you are training to become a medical assistant or a surgeon! It’s not just CPR that saves lives. It’s knowing how to do it correctly. Someone with no formal CPR training could use what they’ve seen on TV to keep some blood flowing. But they may not be able to do it in a way that improves that person’s chance of survival. It’s unlikely you could perform high-quality compressions without some formal training.
It’s not just CPR that saves lives. It’s knowing how to do it correctly. Someone with no formal CPR training could use what they’ve seen on TV to keep some blood flowing. But they may not be able to do it in a way that improves that person’s chance of survival. It’s unlikely you could perform high-quality compressions without some formal training. If you’re a bystander with no medical training, then you may not know how to effectively determine when to start CPR. In a CPR training course, you’ll learn what to look for.
If you’re a bystander with no medical training, then you may not know how to effectively determine when to start CPR. In a CPR training course, you’ll learn what to look for. Doctors classify a severe attack as one that lands you in the emergency room or clinic. But before that happens, someone needs to recognize the person has a severe attack. Here’s what to look for:
Doctors classify a severe attack as one that lands you in the emergency room or clinic. But before that happens, someone needs to recognize the person has a severe attack. Here’s what to look for: If possible, remove the person from the suspected irritant and find somewhere where they can get fresh air. Keep in mind, what you consider fresh air and what this person considers fresh air may be two different things. If this person is allergic to pollen, then taking them outside on a warm spring day may not be the best idea
If possible, remove the person from the suspected irritant and find somewhere where they can get fresh air. Keep in mind, what you consider fresh air and what this person considers fresh air may be two different things. If this person is allergic to pollen, then taking them outside on a warm spring day may not be the best idea Because of their injuries, these patients may experience strokes, heart attacks, internal bleeding, severe burns, and other conditions. Your training helps you identify and respond to these within your nursing capacity.
Because of their injuries, these patients may experience strokes, heart attacks, internal bleeding, severe burns, and other conditions. Your training helps you identify and respond to these within your nursing capacity. Trauma nursing is a rapidly developing area of healthcare. It continues a trend toward specialization.
Trauma nursing is a rapidly developing area of healthcare. It continues a trend toward specialization.
 Synchronized cardioversion is a process to achieve a sinus rhythm in a patient who has arrhythmia. It requires the delivery of a low energy shock at a specific time. Doctors achieve this timing by viewing a defibrillator monitor or using a machine that syncs to the rhythm automatically. In both cases, you’ll only find this equipment in a hospital or specialized clinic.
Synchronized cardioversion is a process to achieve a sinus rhythm in a patient who has arrhythmia. It requires the delivery of a low energy shock at a specific time. Doctors achieve this timing by viewing a defibrillator monitor or using a machine that syncs to the rhythm automatically. In both cases, you’ll only find this equipment in a hospital or specialized clinic.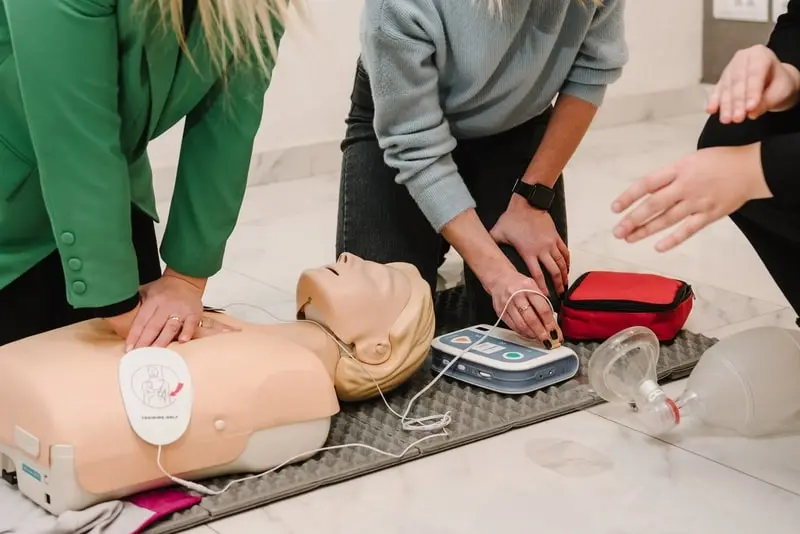 Cardioversion is performed in a hospital with a doctor, an anesthesiologist, and cardiac nursing professionals present. The anesthesiologist will plan and supervise sedation of the patient using general anesthesia. Once sedated, the team performs the following steps:
Cardioversion is performed in a hospital with a doctor, an anesthesiologist, and cardiac nursing professionals present. The anesthesiologist will plan and supervise sedation of the patient using general anesthesia. Once sedated, the team performs the following steps: You may hear a significant amount about synchronized cardioversion vs defibrillation or defibrillation vs synchronized cardioversion. Let’s break down some of the core elements of this comparison of cardioversion vs defibrillation:
You may hear a significant amount about synchronized cardioversion vs defibrillation or defibrillation vs synchronized cardioversion. Let’s break down some of the core elements of this comparison of cardioversion vs defibrillation: In order to understand how to save a life during a cardiac arrest, you need to take a look at the dying process. This begins with the loss of function of a vital organ, e.g., brain, heart, or lungs. If professionals cannot restore this organ, it causes other organ failures.
In order to understand how to save a life during a cardiac arrest, you need to take a look at the dying process. This begins with the loss of function of a vital organ, e.g., brain, heart, or lungs. If professionals cannot restore this organ, it causes other organ failures.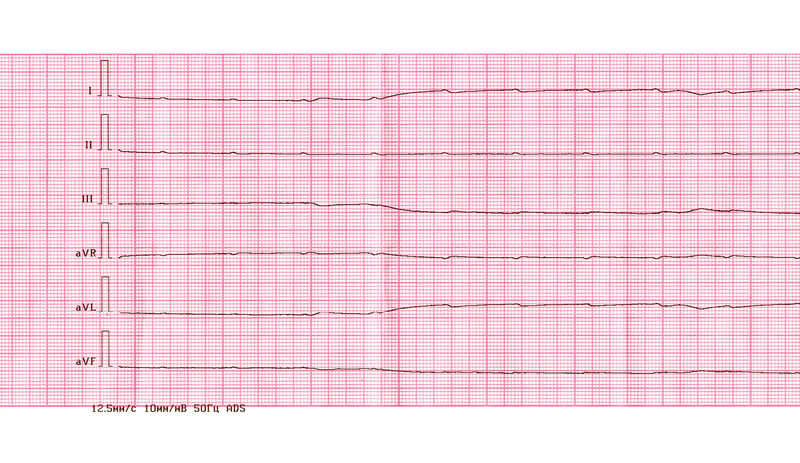 What Does a PEA Look Like on ECG?
What Does a PEA Look Like on ECG?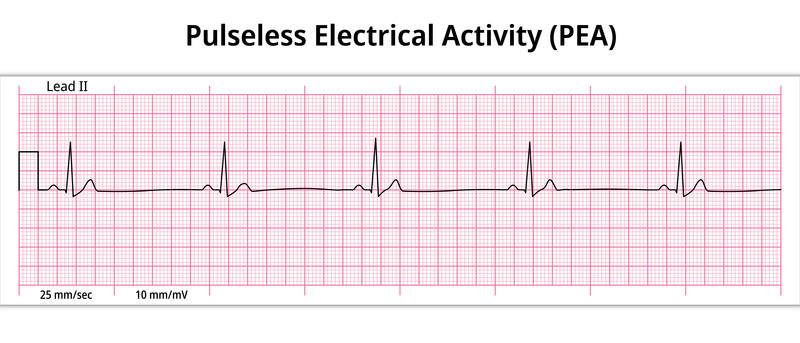 The first step in PEA arrest is action. The only way to know if a heart arrest is occurring as a result of a PEA is through the use of an electrocardiogram. Most of the time, electrocardiograms are not readily available outside of a medical facility, which makes it hard for rescuers to know that a PEA arrest is occurring.
The first step in PEA arrest is action. The only way to know if a heart arrest is occurring as a result of a PEA is through the use of an electrocardiogram. Most of the time, electrocardiograms are not readily available outside of a medical facility, which makes it hard for rescuers to know that a PEA arrest is occurring. For pediatric patients, you have a separate
For pediatric patients, you have a separate  Another study
Another study The evidence is clear. Protocol adherence saves lives. But team leaders and team members don’t always follow the protocol. As a team leader, what can you do about that? We have some tips.
The evidence is clear. Protocol adherence saves lives. But team leaders and team members don’t always follow the protocol. As a team leader, what can you do about that? We have some tips.