Vasopressin vs. Epinephrine in the Treatment of Sudden Cardiac Arrest
VASOPRESSORS, drugs that cause the constriction of blood vessels, are vital, life‐saving drugs used in Advanced Cardiac Life Support (ACLS) protocols. Administration of vasopressors during episodes of low blood pressure result in constriction of blood vessels which shunts blood to the core organs such as heart and brain.
vasopressors during episodes of low blood pressure result in constriction of blood vessels which shunts blood to the core organs such as heart and brain.
It is important to know that a recent study suggests the vasoconstrictive properties of epinephrine may be blunted in respiratory or metabolic acidosis. Vasopressin, another vasopressor, has a comparable effect to epinephrine in return of spontaneous circulation (ROSC), and may maintain its effectiveness in the presence of acidosis.
Current ACLS guidelines indicate that vasopressin may be used as standalone therapy, or after an initial dose of epinephrine. This is because there is no randomized controlled clinical trial proving one agent to be more effective than the other. With this in mind, how can we enhance ACLS drug delivery and improve survival of victims experiencing cardiac arrest?
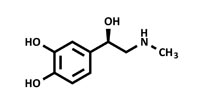 To better understand how you can optimize choosing between epinephrine and vasopressin, it’s crucial to recognize the action of drugs used in the ACLS algorithms and consider individual patient circumstances of cardiac arrest. Epinephrine is an adrenergic agonist, and exerts vasoconstriction by binding to a‐receptors in the peripheral vasculature, which ultimately moves the blood volume to visceral and cerebral regions. Epinephrine also binds to ?‐receptors, improving the contractile state of the heart, stimulating spontaneous contractions. It is important to keep in mind that epinephrine may potentiate ventricular fibrillation. This potential proarrhythmic effect has prompted researchers to look for alternate vasopressors. This is where vasopressin becomes an important drug for ACLS, supporting central organ perfusion by increasing peripheral vascular resistance and increasing arterial blood pressure without increasing or decreasing heart rate.
To better understand how you can optimize choosing between epinephrine and vasopressin, it’s crucial to recognize the action of drugs used in the ACLS algorithms and consider individual patient circumstances of cardiac arrest. Epinephrine is an adrenergic agonist, and exerts vasoconstriction by binding to a‐receptors in the peripheral vasculature, which ultimately moves the blood volume to visceral and cerebral regions. Epinephrine also binds to ?‐receptors, improving the contractile state of the heart, stimulating spontaneous contractions. It is important to keep in mind that epinephrine may potentiate ventricular fibrillation. This potential proarrhythmic effect has prompted researchers to look for alternate vasopressors. This is where vasopressin becomes an important drug for ACLS, supporting central organ perfusion by increasing peripheral vascular resistance and increasing arterial blood pressure without increasing or decreasing heart rate.
A recent study was conducted to determine if vasopressin could improve patient survival when used in combination with epinephrine compared to epinephrine alone. A total of 101 patients who experienced cardiac arrest and required ACLS and vasopressor therapy were reviewed. The results demonstrated no difference in rate of ROSC or survival to hospital discharge when combination vasopressor therapy was utilized. Subgroup analysis did show improved outcomes in cardiac arrest patients with initial arterial pH less than 7.2 who received combination therapy.
The ethics of resuscitation research continue to make randomized clinical trials difficult to conduct, therefore definitive treatments remain elusive. ACLS providers have a responsibility to stay up to date on the latest research and be sure their practice reflects current guidelines. Practitioners should maintain current references and algorithms for quick reference during resuscitations.

