What is ACLS? Your Guide to AMC’s Trusted Certification Courses
What is ACLS? Your Guide to AMC's Trusted Certification Courses

by Greta Kviklyte
Life Saver, AMC
Co-authored by Kim Murray, RN, M.S.
posted on Aug 22, 2024, at 5:22 pm
Understanding the proper procedures to perform Advanced Cardiac Life Support or ACLS is paramount. After all, as a professional in the medical industry, either serving as a nurse, EMT, doctor, or other type of crucial medical care provider, you need to be ACLS certified to ensure that you know what to do should the worst happen.
Drawing on ACLS Certification Training to Save a Life
When answering the question, what is ACLS, your first thought should be how to use this advanced training to save a life. As a medical professional, especially working in the ER, or in critical care, you will find yourself facing life and death decisions on a regular basis.
We offer Online ACLS Certification and Renewal
Your training is what will equip you to react right when seconds matter. Advanced Medical Certification AMC is proudly offering ACLS certification and recertification for you as a busy medical professional to gain important life-saving training.
Answering the Question: What is ACLS?
What is ACLS certification? ACLS, which stands for Advanced Cardiovascular Life Support, is a set of procedures and proven techniques to treat specific, serious medical conditions, like trauma, stroke, shock and cardiac arrest. The end goal of this training is for you, as a medical professional, to be able to effectively stabilize your patient’s dire condition and ultimately restore alertness and vital signs.
ACLS standards are created using evidence-based data that you can commit to memory through your training and then put into practice. This allows you to easily recall these vital skills during moments of intense stress during emergency patient care. ACLS was created initially in 1974 as a way to effectively respond to specific medical emergencies and, in essence, equip you to save lives.
ACLS Certification Teaches Many Actions
After ACLS certification, you will be able to insert an intravenous IV or intraosseous IO line to administer medications and/or fluids, as well as be able to place advanced airways. You will also have a high level of knowledge pertaining to the medications that are used to treat various heart conditions. ACLS skills and essentials are applicable and necessary to provide the best possible treatment for patients in life-threatening conditions involving cardiac-related incidents.
The Importance of ACLS Certification
When you face a situation where your patient is experiencing a medical situation that requires ACLS intervention, it is immensely important that you have the necessary training for a variety of reasons. Proper ACLS implementation will increase a patient’s outcome by ensuring that their neurological function remains intact throughout the cardiovascular event. This sustains life and increases the chances of positive outcomes. The following are some additional reasons why ACLS certification is so important:
- Improves Patient Outcome: When you employ ACLS expertly to save your patient’s life, your quick and effective response potentially minimizes complications and potentially saves lives. In fact, ACLS training (along with additional BLS training) in blue team members, has been proven to significantly improve patient survival and overall discharge rates, according to studies featured in the National Library of Medicine.
- Professional Competence: ACLS certification provides you with the lifesaving skills you need to perform competently when faced with a critical cardiac situation. Once you handle such a situation successfully, you will note a boost in confidence, allowing you to stand tall alongside your colleagues and treat your patients with confidence.
- Standardized Care: There are standards within the medical industry for a reason: they have been proven effective. Therefore, since ACLS follows standardized protocols, you will know you are delivering the right type of care to your patient in distress, facilitating the best outcome.
- Career Advancement: Many healthcare facilities and hospitals require ACLS certification in specific positions. Therefore, for the sake of your career advancement, there are many cases in which you need to obtain your ACLS certification in order to continue expanding your patient care role.
Framework of Protocols For Emergency Patient Care
The ACLS framework is built on protocols formed by clinical studies, patient case studies, opinions of experts in the field, and thorough research. This ACLS response has been set by the International Liaison Committee on Resuscitation (ILCOR). In previous years, the ILCOR released updates to these guidelines once every five years based on their Emergency Cardiovascular Care ECC and Cardiopulmonary Resuscitation CPR.
After 2020, the updates will no longer come in five-year increments but will be maintained consistently and based on up-to-date recommendations. This commitment to consistent updates makes certification and recertification pertaining to ACLS practices much more important and vital to practicing within the medical arena. Therefore, keeping your ACLS certification up-to-date is now more important than ever.
In Classroom Training Vs Online ACLS Certification
When it comes to ACLS certification, there are two main options to obtain these qualifications, those being in classroom training or online learning. At AMC, we offer online training programs that appeal to you as a busy medical professional to get the training you need to make a difference in the medical field. AMC has certified thousands of healthcare providers through its various programs and boasts a 98% national acceptance rate throughout the United States.
Online training offers a measure of flexibility that allows you to work as you go through these courses. It is the same high-quality education, though, as those offered in a more traditional classroom setting. These certifications are based on ILCOR’s standards and guidelines, ensuring accurate training that is accepted by most employers. If your employer does not accept AMC’s ACLS certification, then you can get a refund on their course and certification cost.
Learning How to Implement an ACLS Algorithm
Your ACLS certification course through AMC will cover a wide range of skills necessary to save your patients’ lives. Part of this course is mastering ACLS algorithms, which help you treat those facing cardiac arrest. There is a great need for you to train in these standards of care because cardia arrests are an ever-growing problem. In fact, according to the Sudden Cardiac Arrest Foundation, there were around 356,000 cardiac arrests throughout the United States in 2022. This number showcases the vital need to understand and perfect ACLS algorithms, such as recognizing stroke, heart attack, and acute coronary symptoms and being able to take vital next steps.
Additional Certifications like BLS and PALS
AMC offers additions to ACLS certification, including BLS and PALS certification. BLS stands for Basic Life Support. It is a level of medical care that is used for patients who are facing injuries or life-threatening conditions. It, too, follows the ILCOR’s guidelines for recognizing and treating life-threatening emergencies like CPR and the use of an automated external defibrillator or AED.
PALS, which stands for Pediatric Advanced Life Support, includes basic life support created to manage critically ill children and infants. It is often a good idea when you could be called on to treat a child, such as working as a pediatric care provider, EMT, a critical care professional, ER personnel, or other type of emergency responder.
How BLS and ACLS Certification Differ
There is a great deal of difference between BLS certification and ACLS certification. BLS focuses on basic life-saving techniques, which include common practices like AEO and CPR. ACLS goes deeper and explores more complex and advanced forms of cardiovascular life support. This includes training in advanced airway management, complex resuscitation algorithms, and attention to pharmacology detail. Generally, BLS is aimed at a wider audience in terms of those who might take such a course. BLS can even be applicable to laypersons, while ACLS is specifically designed for you as a medical professional. The following are a few more applicable ways that these two certifications differ, though BLS certification can also be obtained through AMC:
- Training Focus: ACLS focuses on advanced life support training techniques including complex resuscitation algorithms, advanced airway management, and medication management in an emergency situation. On the other hand, BLS focuses on basic life-saving strategies, as outlined above, including AED use, CPR, and choking management.
- Target Audience: ACLS is designed for you as a medical professional who will be put in life-saving situations regularly. BLS is also applicable to you but can also appeal to laypersons who want to know basic life-saving actions.
- Course-Requirements: ACLS certification often requires a BLS certification as well to qualify or as part of ACLS certification. However, BLS certification typically has no prerequisites for entrance.
Your ACLS Certification Exam
The ACLS Certification Exam requires a passing score of 80% and this exam encompasses 50 exam questions. You must pass this to get your certification. Don’t worry if you have to go at a slower pace, as you can save your exam and finish at your convenience. After successfully passing, you can access your digital card instantly or request a certificate or a printed card.
Thankfully, even if you don’t pass the exam initially, you can take the test again as many times as needed to pass. This means there is no need for you to fear not passing as you have numerous chances. Take advantage of the additional resources through AMC to find success. You can also try taking the ACLS certification practice test to see if you are ready.
Tips to Pass Your ACLS Certification
You want to perfect your skills and ensure that you are ready to go back into an emergency situation and do your job to perfection. The first step of this is studying to pass this all-important exam. Thankfully, there are many helpful tips that you can use to increase your chances of success through taking your AMC course. This includes the following easy-to-follow tips:
- Study the Algorithms: As mentioned above, learning the ACLS algorithms is a vital part of mastering your ACLS training.
- Create Graphs and Flowcharts: AMC offers handbooks to help you study, but you can also create your own flowcharts, graphs, or notecards to learn hard-to-remember information.
- Carefully Study ACLS Drugs: As you will learn, medications can make a immense difference when trying to save a life. Part of getting your ACLS certification involves memorizing these drugs, what they do, and any potential side effects to look out for when administering them.
- Utilize Review Tools: Take advantage of online review tools or practice tests through AMC to study for your exam before taking it.
- Study Daily: Although you are likely busy and trying hard to take in a great deal of new information, it’s important to study regularly, ideally on a daily basis, in order to commit your new training to memory.
Advance Your Skills with AMC’s ACLS Certification
Ready to enhance your medical expertise and save lives? Enroll in AMC’s ACLS Certification course today and ensure you’re fully equipped with the life-saving skills needed in critical moments. Our flexible online training allows you to learn at your own pace, providing you with the tools and confidence to perform with excellence in any emergency situation. Don’t wait – advance your career and make a difference now.
FAQS About ACLS Certification Through AMC
In addition to answering the all-important question of what is ACLS, this informative FAQ section will go over all sorts of common questions pertaining to AMC’s ACLS certification course:
What About ACLS Recertification?
ACLS certification is necessary to work in a variety of medical environments. However, getting this certification once doesn’t mean you are certified for life. In reality, due to the ever-changing nature of the medical profession, having such a certification that never expires would not be a good idea anyway. Your ACLS certification at AMC is valid for two years.
After that time, you can get recertified in ACLS, ensuring they are up-to-date with any new procedures and building on the training you already have in place. This is immensely important in the ever-evolving medical field that is always changing with the introduction of innovative technologies and life-saving methods. Of course, AMC does offer ACLS for Life, which is another option for certification that might be advantageous for you.
What is ACLS For Life?
AMC offers a unique option for you if you plan to remain in the medical field for life, called ACLS for Life certification. This doesn’t mean that you don’t have to retest after two years to get your updated certification. This is still necessary. However, the difference is that you only have to pay once. This increased amount you pay with the Life version means you can retest and receive your digital card of certification every two years for life!
How Many Medical Professionals Have Used AMC?
At the time of publishing, there were over 220,000 medical professionals who have been certified through AMA. There is a full money-back guarantee and your AMC’s ACLS certification is accepted nationwide. You can also get up to eight AMA category 1 credits as part of this course.
Why Choose AMC For Your ACLS Certification or Recertification?
At AMC, we offer a money-back guarantee if a company does not accept the AMC ACLS certification (though this is unlikely to happen). This comprehensive course allows you to complete your ACLS certification and choose adds-on’s to this certification like BLS and PALS certification.
You can also choose the ACLS for life as outlined above if you plan to remain in the medical profession for the duration of your career. This can save you a great deal of money over time and keep you certified every two years throughout your career.





 position of the patient just right,
position of the patient just right,  The patient has a suspected upper airway obstruction and is unresponsive
The patient has a suspected upper airway obstruction and is unresponsive AED, and First Aid online training course. This course covers key areas such as administering CPR, using AED devices, and
AED, and First Aid online training course. This course covers key areas such as administering CPR, using AED devices, and CPR algorithms
CPR algorithms

 In the event of cardiac arrest or stroke, immediate intervention makes a huge difference. This is why it’s so important to recognize the initial symptoms so you can spring into action sooner rather than later.
In the event of cardiac arrest or stroke, immediate intervention makes a huge difference. This is why it’s so important to recognize the initial symptoms so you can spring into action sooner rather than later.




 Instead, ACLS protocols are more like a tree with branches. You choose to take a branch by asking certain questions about the person’s condition and using
Instead, ACLS protocols are more like a tree with branches. You choose to take a branch by asking certain questions about the person’s condition and using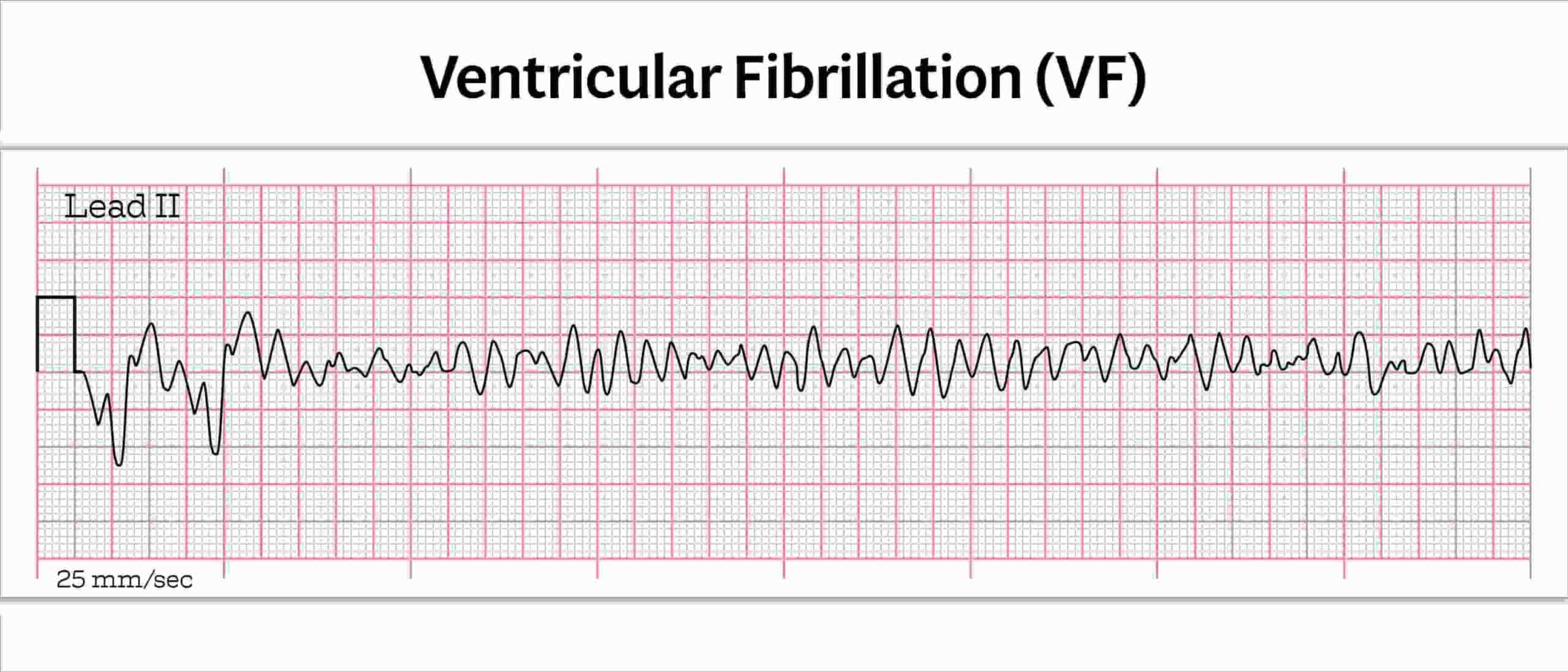
 The “or” is important here because if there were only “no pulse”, that could be a shockable rhythm, VTach (described above). It’s important to put all of the pieces together.
The “or” is important here because if there were only “no pulse”, that could be a shockable rhythm, VTach (described above). It’s important to put all of the pieces together. However, asystole can also include slight movement from a flatline. In fact, a complete flatline is uncommon because ventilation and chest compression efforts can make blips appear on the readout.
However, asystole can also include slight movement from a flatline. In fact, a complete flatline is uncommon because ventilation and chest compression efforts can make blips appear on the readout.