- BLS for Children 1 – Puberty
- One & Two Rescuer BLS for Children
- Pediatric BLS Algorithm
- Child Ventilation
Pediatric BLS Algorithm
Knowing the pediatric BLS algorithm can make a critical difference in patient outcomes in emergency situations involving infants and children. This guide provides healthcare professionals and first responders with a step-by-step approach to delivering high-quality basic life support (BLS) pediatric patients.
Understanding the Pediatric BLS Algorithm
The pediatric BLS algorithm is a structured sequence of actions designed to assist rescuers in assessing and managing life-threatening emergencies in infants (under one year) and children (from 1 year to puberty). It emphasizes early recognition, effective chest compressions, timely ventilations, and automated external defibrillators (AEDs) when appropriate.
Pediatric Basic Life Support Algorithm
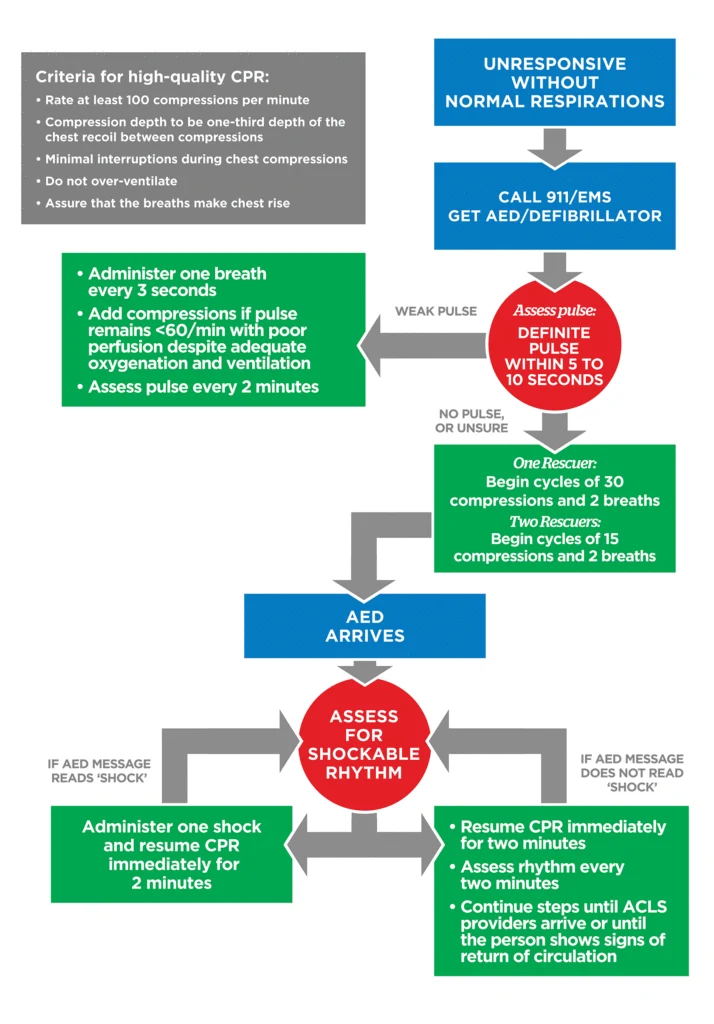
Figure 9
Key Steps of the Pediatric BLS Algorithm
1. Ensure Scene Safety
Before approaching the patient, ensure the environment is safe for you and the victim.
2. Check Responsiveness
Gently tap the child and shout to see if they respond. For infants, tap the bottom of the bare foot.
3. Activate Emergency Response
- If you are alone and the collapse was unwitnessed:
- Perform 2 minutes of CPR before calling emergency services.
- If you are not alone, send someone to activate the emergency response system and retrieve an AED immediately. If alone and unable to call EMS, Perform 2 minutes of CPR before leaving the scene to call EMS.
- Send someone to activate the emergency response system and retrieve an AED immediately.
4. Assess Breathing and Pulse
- Breathing:
- Look for normal breathing (not gasping).
- Pulse:
- Check the brachial pulse in infants or carotid/femoral pulse in children for no more than 10 seconds.
5. Begin High-Quality CPR
If there is no breathing or only gasping and no pulse (or a pulse less than 60 bpm with signs of poor perfusion), start CPR immediately.
Chest Compressions:
- Infants:
- Use two fingers in the center of the chest, just below the nipple line.
- Children:
- Use one or two hands (depending on the child’s size) on the sternum’s lower half.
Compression Depth:
- At least one-third the depth of the chest (about 1.5 inches/4 cm for infants, 2 inches/5 cm for children).
- Rate:
- 100 to 120 compressions per minute.
- Allow full chest recoil after each compression.
Ventilations:
- Open the airway using the head-tilt-chin-lift method.
- Give two breaths after every 30 compressions if you’re alone or after every 15 compressions if there are two rescuers.
- Each breath should last about 1 second, making the chest rise visibly.
6. Use of AED
- Attach the AED as soon as it is available.
- Pediatric Pads:
- Use if the child is less than eight years old.
- If Pediatric Pads Are Unavailable:
- Use adult pads, ensuring they do not touch each other.
- Follow the AED prompts and deliver shocks if advised.
7. Continue CPR
Resume CPR immediately after the AED delivers a shock or if no shock is advised. Rotate compressors every 2 minutes to prevent fatigue.
Importance of Early Intervention
Timely and effective application of the pediatric BLS algorithm significantly improves survival rates and neurological outcomes. Children have unique anatomical and physiological characteristics, making specialized pediatric BLS training essential for proper care.
Enhance Your Skills with Our Online BLS Certification Course
Stay prepared for pediatric emergencies by enrolling in our Online BLS Certification Course. The course offers comprehensive training on the pediatric BLS algorithm, ensuring you are equipped with the latest lifesaving techniques.
Course Benefits:
- Comprehensive Curriculum: Covers BLS protocols for infants, children, and adults.
- Flexible Learning: Access course materials anytime, anywhere.
- Accredited Certification: Earn a certification recognized across health care institutions.
- Instant Certificate: Receive your digital certificate immediately upon completion.
- Continuing Education Credits: Fulfill your professional development requirements.
Stay Informed and Prepared
Regular practice and staying current with the pediatric BLS algorithm are vital for effective emergency response. Enhancing your skills improves patient outcomes and demonstrates a commitment to your professional role.


